Hirschsprung’s Disease, often abbreviated as HD, is a rare congenital condition that affects the large intestine and causes problems with passing stool. This condition occurs when certain nerve cells are missing from parts of the colon, leading to a lack of proper muscle contractions needed for bowel movements. In this article, we will explore the details of Hirschsprung’s Disease, including its symptoms, diagnostic methods, and treatment options.
Overview of Hirschsprung’s Disease
Hirschsprung’s Disease is a birth defect that primarily affects the digestive system. It occurs during fetal development when the nerve cells that are supposed to grow along the walls of the colon do not develop properly. These nerve cells, called ganglion cells, are essential for controlling the muscles in the intestines. Without them, the affected part of the colon cannot relax, leading to a blockage that prevents stool from passing through.
This condition is present at birth but may not always be diagnosed immediately. It is more common in boys than girls and tends to occur more frequently in children with other genetic conditions, such as Down syndrome. The severity of the disease can vary depending on how much of the colon is affected.
Causes of Hirschsprung’s Disease
The exact cause of Hirschsprung’s Disease is not fully understood, but it is believed to result from a combination of genetic and environmental factors. Research has shown that mutations in certain genes play a role in the development of the condition. These genetic changes can be inherited or occur spontaneously during fetal development.
In some cases, Hirschsprung’s Disease runs in families, suggesting a hereditary component. If one child in a family has the condition, there is an increased risk that future siblings may also be affected. However, most cases occur in families with no prior history of the disease.
Symptoms of Hirschsprung’s Disease
The symptoms of Hirschsprung’s Disease typically appear shortly after birth, although they can sometimes go unnoticed until later in childhood. The severity and timing of symptoms depend on how much of the colon is affected. Common signs include:
- Failure to pass meconium: Meconium is the first stool that newborns pass, usually within the first 24 to 48 hours of life. Infants with Hirschsprung’s Disease often fail to pass meconium within this timeframe.
- Swollen abdomen: Due to the buildup of stool in the colon, the abdomen may appear swollen or distended.
- Vomiting: Infants may vomit, sometimes with bile, as a result of the intestinal blockage.
- Constipation: Chronic constipation is a hallmark symptom, with some children experiencing infrequent bowel movements or difficulty passing stool.
- Poor feeding: Infants may show signs of poor feeding, irritability, or failure to thrive due to discomfort and nutritional deficiencies.
In older children, symptoms may include chronic constipation that does not improve with standard treatments, recurrent episodes of abdominal pain, and poor growth. In severe cases, complications such as enterocolitis, a serious infection of the intestines, can occur.
Diagnosis of Hirschsprung’s Disease
Diagnosing Hirschsprung’s Disease involves a combination of physical examinations, medical history reviews, and specialized tests. Early diagnosis is crucial to prevent complications and ensure timely treatment. The following methods are commonly used:
Physical Examination
A healthcare provider may suspect Hirschsprung’s Disease based on symptoms such as a swollen abdomen, failure to pass stool, or chronic constipation. During a physical examination, the doctor may feel the abdomen for signs of blockage or perform a digital rectal exam to assess the tone of the rectum.
Diagnostic Tests
To confirm the diagnosis, several tests may be conducted:
- Abdominal X-ray: An X-ray can reveal signs of intestinal blockage or a dilated colon.
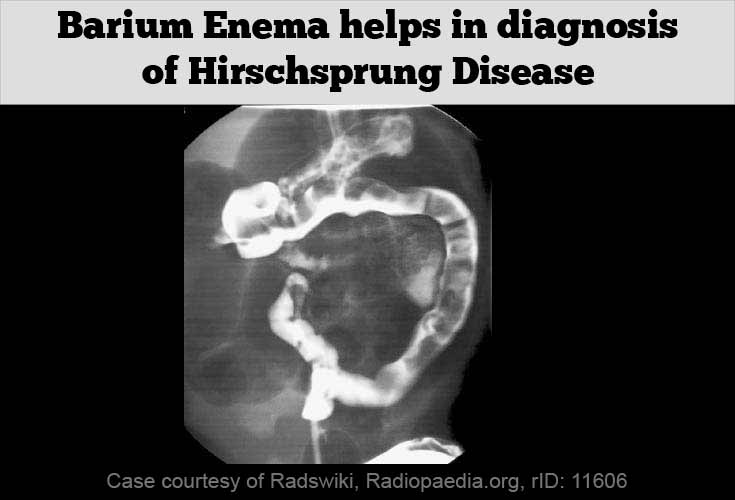
- Contrast enema: This imaging test involves inserting a contrast dye into the rectum to highlight the structure of the colon. It can help identify areas where the colon is narrowed or enlarged.
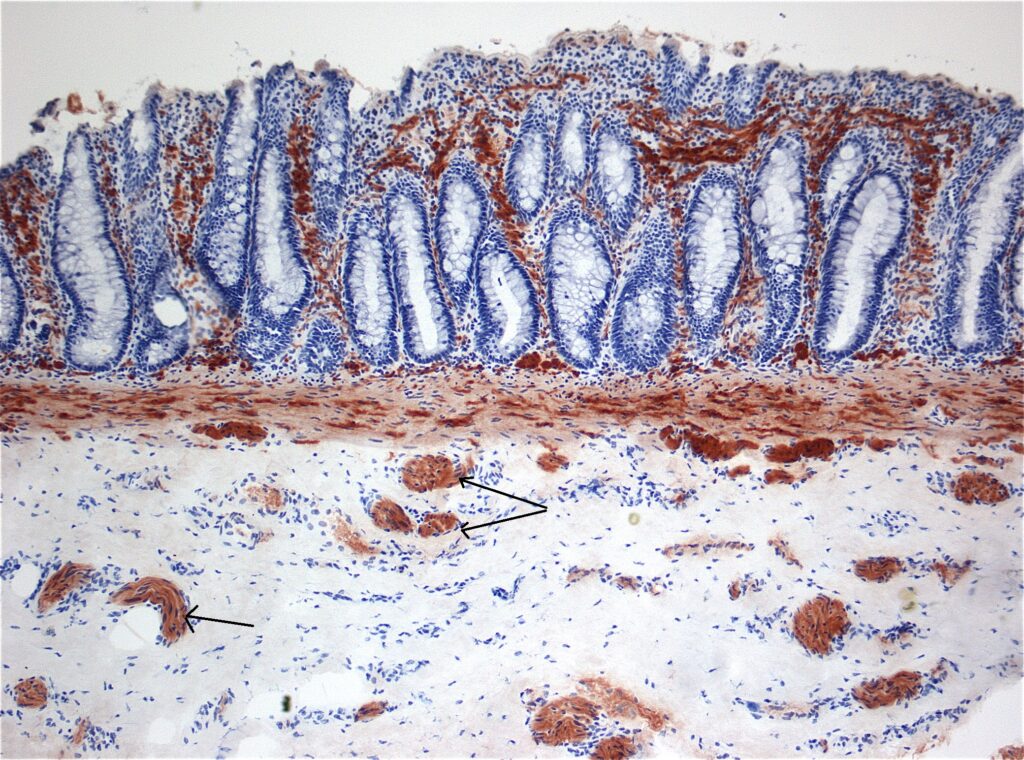
- Rectal biopsy: A small sample of tissue is taken from the rectum and examined under a microscope. The absence of ganglion cells confirms the diagnosis of Hirschsprung’s Disease.
- Anorectal manometry: This test measures the pressure and muscle contractions in the rectum and anus. In children with Hirschsprung’s Disease, the muscles in the affected area do not relax properly.
These tests help doctors determine the extent of the affected area in the colon and plan appropriate treatment.
Treatment Options for Hirschsprung’s Disease
The primary goal of treatment for Hirschsprung’s Disease is to remove the portion of the colon that lacks nerve cells and restore normal bowel function. Treatment options vary depending on the severity of the condition and the age of the patient.
Surgical Treatment
Surgery is the mainstay of treatment for Hirschsprung’s Disease. There are several surgical procedures available, and the choice depends on the length of the affected colon and the overall health of the child.
- Pull-through procedure: This is the most common surgery for Hirschsprung’s Disease. During the procedure, the surgeon removes the diseased portion of the colon and connects the healthy part directly to the anus. This allows stool to pass normally.
- Ostomy surgery: In some cases, especially when the child is very ill or the colon is severely affected, a temporary ostomy may be performed. This involves creating an opening in the abdomen to allow stool to exit the body into a bag. Once the child’s condition improves, a second surgery is performed to complete the pull-through procedure.
Most surgeries for Hirschsprung’s Disease are successful, and children can lead normal lives afterward. However, some may experience complications such as constipation, diarrhea, or incontinence, which require ongoing management.
Non-Surgical Management
In mild cases or while awaiting surgery, non-surgical approaches may be used to manage symptoms:
- Enemas: Regular enemas can help clear the colon of stool and relieve symptoms of blockage.
- Dietary changes: A high-fiber diet and adequate hydration can help soften stools and make bowel movements easier.
- Laxatives: In some cases, medications may be prescribed to promote bowel movements.
However, these measures are typically temporary solutions and do not address the underlying cause of the condition.
Complications of Hirschsprung’s Disease
If left untreated, Hirschsprung’s Disease can lead to serious complications. Some of the most common complications include:
- Enterocolitis: This is a potentially life-threatening infection of the intestines that can cause fever, diarrhea, and dehydration. Prompt medical attention is required to treat this condition.
- Bowel perforation: The buildup of stool and gas in the colon can cause the intestinal wall to rupture, leading to peritonitis, a severe infection of the abdominal cavity.
- Growth delays: Chronic constipation and poor nutrient absorption can result in delayed growth and development in children.
Early diagnosis and treatment are essential to prevent these complications and ensure the best possible outcome for affected individuals.
Living with Hirschsprung’s Disease
Children who undergo surgery for Hirschsprung’s Disease often experience significant improvement in their symptoms. However, ongoing care and monitoring may be necessary to address any lingering issues, such as bowel control problems or recurrent constipation. Parents and caregivers play a vital role in supporting the child’s recovery and helping them adapt to any lifestyle changes.
Regular follow-up appointments with a pediatric gastroenterologist are important to monitor the child’s progress and address any concerns. In addition, education about the condition and its management can empower families to provide the best care for their child.