Hypernatremia, commonly referred to as high sodium levels in the blood, is a medical condition that occurs when there is an imbalance in the concentration of sodium relative to water in the body. This condition can have serious implications if left untreated, making it essential to understand its causes, symptoms, and proper care strategies. In this article, we will delve into the details of what leads to elevated sodium levels, how it manifests in the body, and what steps can be taken to manage and prevent it.
Understanding Sodium and Its Role in the Body
Sodium is one of the most important electrolytes in the human body. It plays a critical role in maintaining fluid balance, supporting nerve function, and aiding muscle contractions. The kidneys are primarily responsible for regulating sodium levels by adjusting how much is excreted in urine. When sodium levels rise too high, it disrupts the delicate balance necessary for optimal bodily functions.
What Happens When Sodium Levels Are Too High?
When sodium levels in the blood become excessively high, it creates a state of dehydration within the cells. Water moves out of the cells to balance the high sodium concentration in the bloodstream, causing the cells to shrink. This process can affect multiple organs, particularly the brain, leading to a range of symptoms and potential complications.
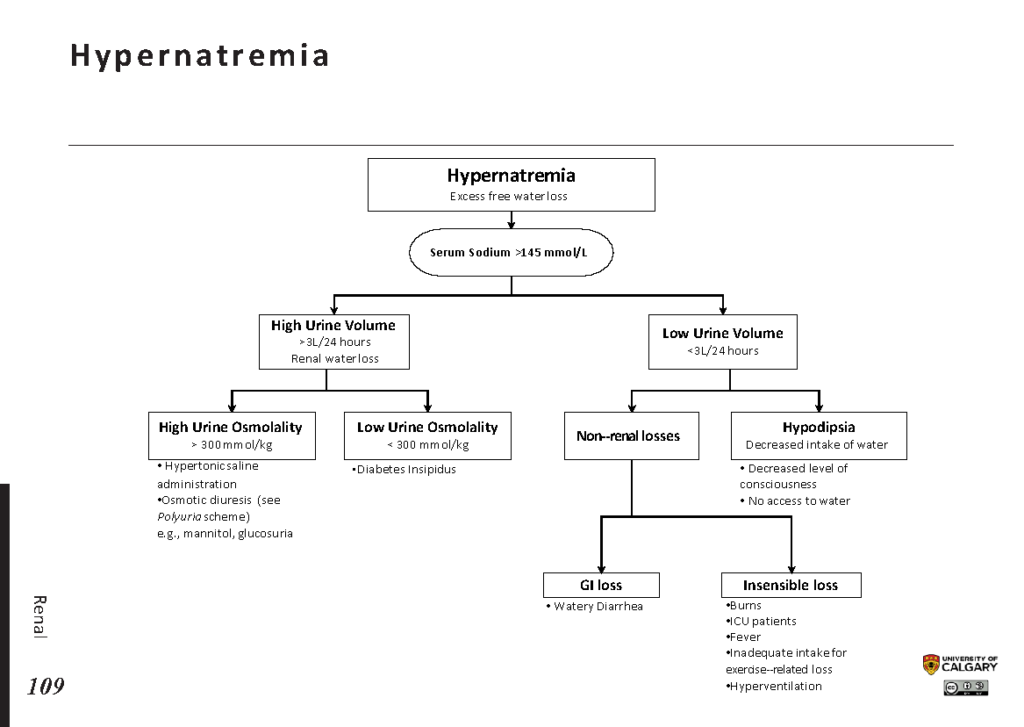
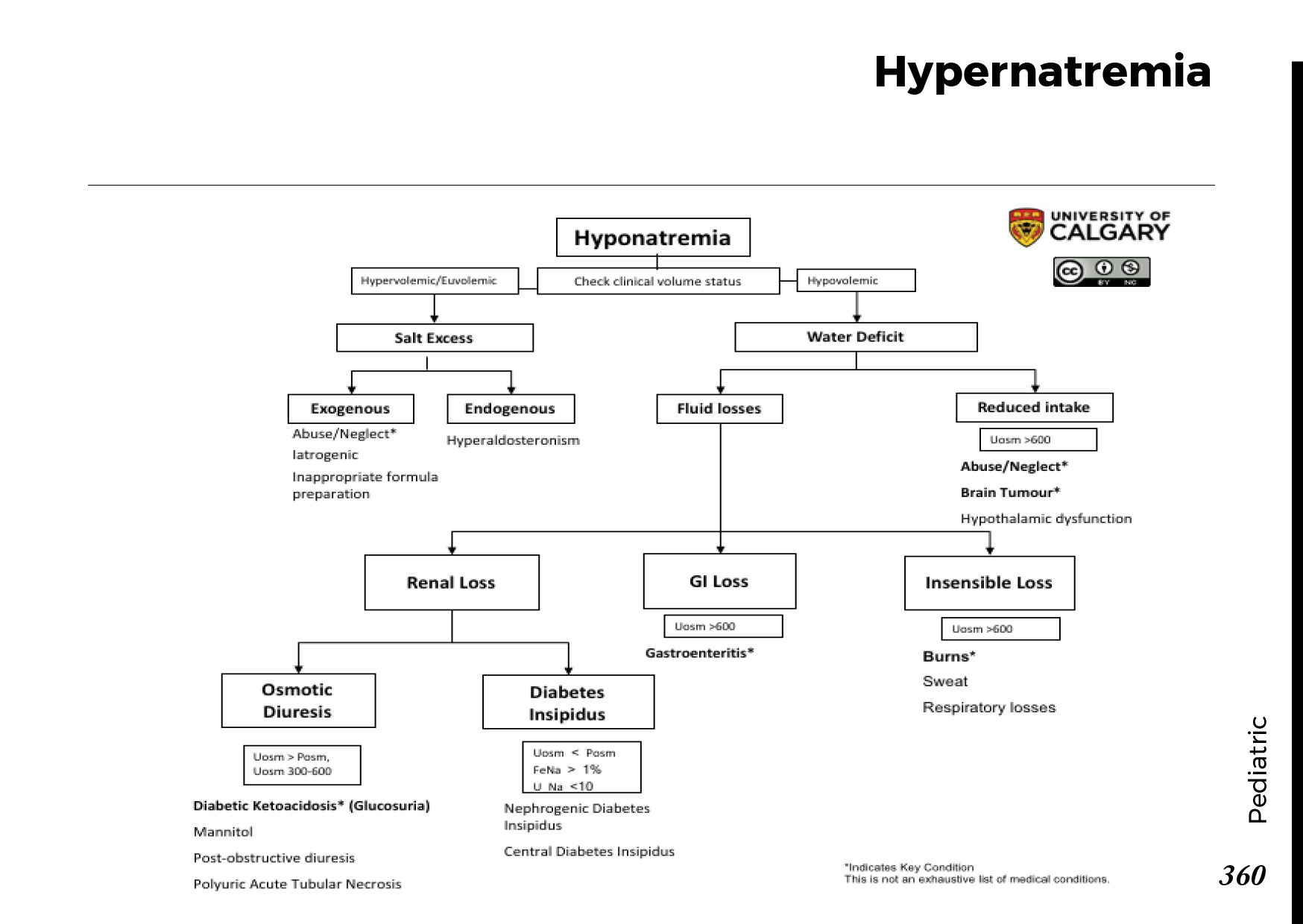
Causes of Elevated Sodium Levels
There are several factors that can contribute to elevated sodium levels in the blood. These causes can be broadly categorized into issues related to water loss, excessive sodium intake, or underlying medical conditions.
Excessive Loss of Water
- Dehydration: One of the most common causes of elevated sodium levels is dehydration. This can occur due to inadequate fluid intake, excessive sweating, vomiting, diarrhea, or the use of diuretics.
- Burns and Skin Injuries: Severe burns or skin injuries can lead to significant water loss through damaged tissues, contributing to an imbalance in sodium levels.
- Diabetes Insipidus: This condition affects the body’s ability to regulate water balance, often resulting in excessive urination and subsequent dehydration.
Excessive Sodium Intake
- High Salt Consumption: Consuming large amounts of salt, either through diet or intravenous fluids, can overwhelm the body’s ability to maintain sodium balance.
- Medical Treatments: Certain medical treatments, such as hypertonic saline infusions, can inadvertently raise sodium levels if not carefully monitored.
Underlying Medical Conditions
- Kidney Disorders: Conditions like chronic kidney disease can impair the kidneys’ ability to excrete excess sodium.
- Hormonal Imbalances: Disorders affecting hormones that regulate sodium and water balance, such as aldosterone or antidiuretic hormone imbalances, can lead to elevated sodium levels.
- Feeding Tubes or Intravenous Nutrition: Patients receiving nutrition through feeding tubes or intravenous methods may experience imbalances if the fluids are not properly formulated.
Symptoms of Elevated Sodium Levels
The symptoms of high sodium levels can vary depending on the severity of the imbalance and how quickly it develops. Acute cases tend to produce more severe symptoms, while chronic cases may present with milder signs.
Mild to Moderate Symptoms
- Increased thirst
- Dry mouth and mucous membranes
- Fatigue and weakness
- Decreased urination
- Muscle twitching or spasms
Severe Symptoms
- Confusion and disorientation
- Agitation or irritability
- Seizures
- Coma
In severe cases, the brain can be significantly affected due to cellular dehydration, leading to life-threatening complications. Prompt medical attention is crucial to prevent permanent damage.
Diagnosis of Elevated Sodium Levels
Diagnosing elevated sodium levels typically involves a combination of clinical evaluation, patient history, and laboratory tests. Healthcare providers will assess symptoms, inquire about fluid intake and losses, and review any medications or medical conditions that could contribute to the imbalance.
Laboratory Tests
- Blood Tests: A basic metabolic panel or serum electrolyte test can measure sodium levels in the blood.
- Urine Tests: Analyzing urine concentration and sodium content can help determine whether the issue stems from excessive sodium intake or water loss.
Additional Evaluations
- Imaging studies, such as MRI or CT scans, may be used if neurological symptoms are present to rule out other causes.
- Hormone level tests may be conducted to identify any underlying endocrine disorders.
Treatment and Management of Elevated Sodium Levels
Treatment for elevated sodium levels focuses on addressing the underlying cause, restoring fluid balance, and preventing complications. The approach depends on the severity of the condition and the patient’s overall health.
Restoring Fluid Balance
Rehydration is the cornerstone of treatment for elevated sodium levels. This can be achieved through oral fluids or intravenous administration, depending on the patient’s condition.
- Oral Rehydration: For mild cases, increasing water intake or consuming electrolyte solutions can help restore balance.
- Intravenous Fluids: In severe cases, healthcare providers may administer hypotonic fluids, such as half-normal saline or dextrose solutions, to gradually lower sodium levels.
Addressing Underlying Causes
Identifying and treating the root cause of elevated sodium levels is essential for long-term management. This may involve:
- Adjusting medications that contribute to fluid loss, such as diuretics.
- Treating underlying medical conditions, such as kidney disorders or hormonal imbalances.
- Modifying dietary habits to reduce sodium intake.
Monitoring and Follow-Up
Patients with elevated sodium levels require close monitoring to ensure that sodium levels return to normal without causing complications. Rapid correction of sodium levels can lead to a dangerous condition known as osmotic demyelination syndrome, which affects the brain. Therefore, healthcare providers aim for a gradual reduction in sodium levels over 24 to 48 hours.
Preventing Elevated Sodium Levels
Prevention is key to avoiding the complications associated with elevated sodium levels. By adopting healthy habits and being mindful of risk factors, individuals can reduce their chances of developing this condition.
Staying Hydrated
Maintaining adequate fluid intake is one of the simplest ways to prevent elevated sodium levels. Drinking water regularly, especially during hot weather or physical activity, helps ensure proper hydration.
Managing Sodium Intake
Reducing dietary sodium can help prevent excessive accumulation in the bloodstream. This includes:
- Avoiding processed and packaged foods, which are often high in salt.
- Using herbs and spices instead of salt to flavor meals.
- Reading food labels to monitor sodium content.
Regular Health Check-Ups
Individuals with chronic medical conditions, such as kidney disease or diabetes, should undergo regular check-ups to monitor sodium levels and address any imbalances early.
Caring for Someone With Elevated Sodium Levels
If you are caring for someone with elevated sodium levels, it is important to provide support and ensure they follow their treatment plan. Here are some tips for caregivers:
- Encourage the person to drink plenty of fluids, unless otherwise advised by a healthcare provider.
- Monitor for signs of worsening symptoms, such as confusion or seizures, and seek medical help immediately if they occur.
- Assist with dietary changes by preparing low-sodium meals and snacks.
- Keep track of medications and ensure they are taken as prescribed.
Conclusion
Elevated sodium levels in the blood can have serious consequences if not properly managed. By understanding the causes, recognizing the symptoms, and following appropriate care strategies, individuals can take proactive steps to maintain their health and well-being.