Dyslipidemia, commonly known as high cholesterol and triglycerides, is a medical condition that affects millions of people worldwide. It occurs when there is an imbalance in the levels of lipids, such as cholesterol and triglycerides, in the blood. This imbalance can lead to serious health complications if left untreated. Understanding this condition, its causes, how it is diagnosed, and the ways it can be managed is crucial for maintaining good cardiovascular health.
What is Dyslipidemia?
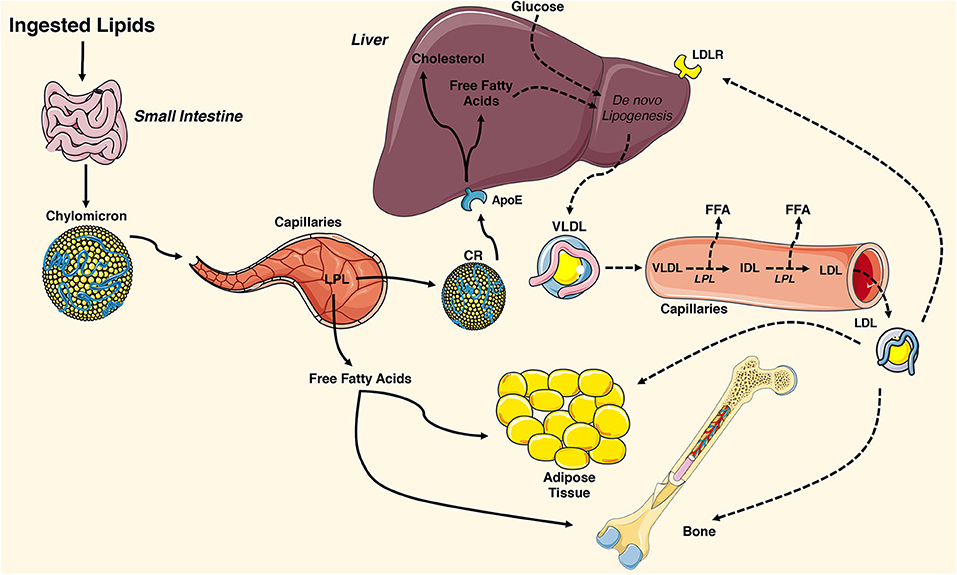
Dyslipidemia refers to abnormal levels of lipids in the bloodstream. Lipids are fats or fat-like substances that are essential for various bodily functions, including energy storage and cell membrane formation. The two primary types of lipids involved in dyslipidemia are cholesterol and triglycerides. When these substances are present in excessive amounts, they can accumulate in the walls of arteries, leading to atherosclerosis, a condition characterized by the hardening and narrowing of arteries.
Types of Lipids Involved
- Cholesterol: A waxy substance found in all cells of the body. It is necessary for producing hormones, vitamin D, and substances that help digest food. However, too much cholesterol can be harmful.
- Triglycerides: A type of fat found in the blood. The body uses triglycerides for energy, but high levels can increase the risk of heart disease.
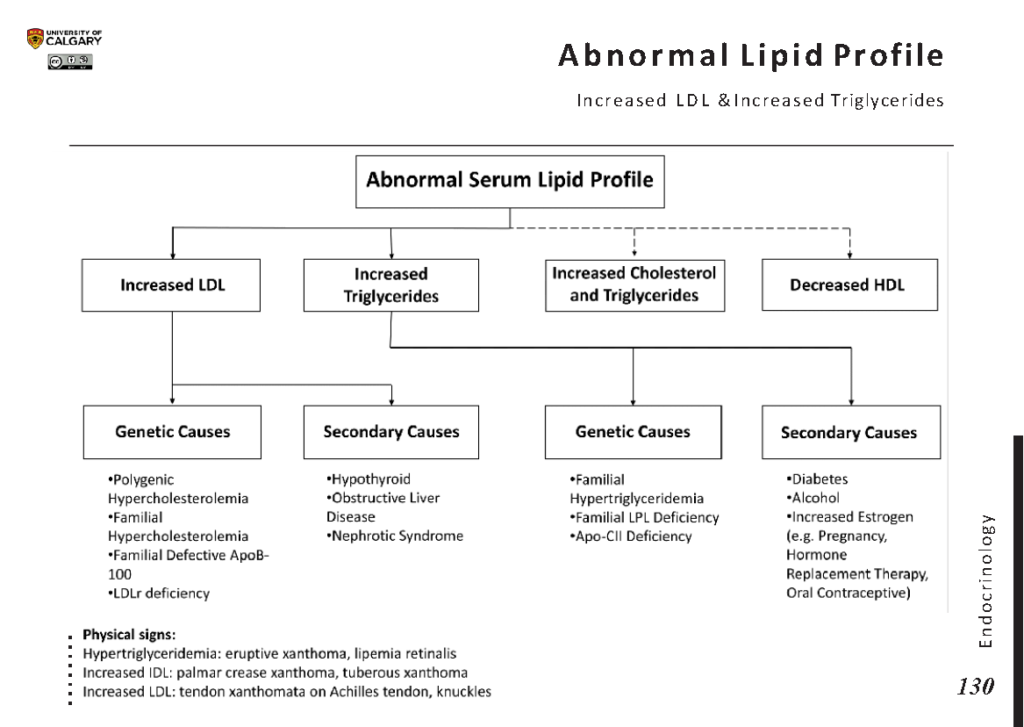
Causes of Dyslipidemia
The development of dyslipidemia can be attributed to a combination of genetic, lifestyle, and medical factors. Understanding these causes is key to preventing and managing the condition effectively.
Genetic Factors
Some individuals inherit genes that predispose them to high cholesterol or triglyceride levels. Familial hypercholesterolemia is one such genetic condition where the body is unable to remove excess cholesterol from the blood, leading to dangerously high levels.
Lifestyle Factors
Unhealthy lifestyle choices play a significant role in the development of dyslipidemia. These include:
- Poor Diet: Consuming foods high in saturated fats, trans fats, and cholesterol can raise lipid levels.
- Lack of Physical Activity: Sedentary behavior can lower the levels of high-density lipoprotein, often referred to as “good” cholesterol.
- Obesity: Excess body weight is associated with higher levels of triglycerides and lower levels of good cholesterol.
- Smoking: Smoking reduces the levels of good cholesterol and damages blood vessels, increasing the risk of heart disease.
- Excessive Alcohol Consumption: Drinking too much alcohol can raise triglyceride levels and contribute to other health problems.
Medical Conditions
Certain medical conditions can also lead to dyslipidemia. These include:
- Diabetes: Poorly controlled diabetes can lead to high triglyceride levels and low levels of good cholesterol.
- Hypothyroidism: An underactive thyroid gland can cause elevated cholesterol levels.
- Kidney Disease: Chronic kidney disease can disrupt lipid metabolism, leading to dyslipidemia.
- Liver Disease: Liver dysfunction can impair the body’s ability to process lipids properly.
How is Dyslipidemia Diagnosed?
Diagnosing dyslipidemia typically involves a series of tests and evaluations to assess lipid levels and identify any underlying causes. Early detection is crucial for preventing complications.
Blood Tests
A lipid profile, also known as a lipid panel, is the primary test used to diagnose dyslipidemia. This test measures the following:
- Total Cholesterol: The total amount of cholesterol in the blood.
- Low-Density Lipoprotein: Often referred to as “bad” cholesterol, high levels can lead to plaque buildup in arteries.
- High-Density Lipoprotein: Known as “good” cholesterol, it helps remove cholesterol from the bloodstream.
- Triglycerides: High levels are associated with an increased risk of heart disease.
Additional Evaluations
In some cases, additional tests may be required to determine the underlying cause of dyslipidemia. These may include:
- Thyroid Function Tests: To check for hypothyroidism.
- Blood Sugar Tests: To evaluate for diabetes or insulin resistance.
- Liver Function Tests: To assess liver health.
- Kidney Function Tests: To evaluate kidney health.
Managing Dyslipidemia
Effective management of dyslipidemia involves a combination of lifestyle changes, medications, and regular monitoring. The goal is to reduce the risk of cardiovascular disease and improve overall health.
Lifestyle Modifications
Making healthy lifestyle choices is the cornerstone of managing dyslipidemia. These changes not only help lower lipid levels but also improve overall well-being.
Dietary Changes
A heart-healthy diet is essential for managing dyslipidemia. Key dietary recommendations include:
- Reduce Saturated and Trans Fats: Limit intake of red meat, full-fat dairy products, and processed foods.
- Increase Fiber Intake: Foods rich in soluble fiber, such as oats, beans, and fruits, can help lower cholesterol levels.
- Eat More Fruits and Vegetables: These are rich in antioxidants and nutrients that support heart health.
- Choose Healthy Fats: Opt for sources of unsaturated fats, such as olive oil, avocados, and nuts.
- Limit Alcohol and Sugary Beverages: These can contribute to high triglyceride levels.
Physical Activity
Regular exercise is beneficial for improving lipid profiles. Engaging in at least 150 minutes of moderate-intensity aerobic activity per week, such as brisk walking or cycling, can help raise good cholesterol levels and lower triglycerides.
Weight Management
Maintaining a healthy weight is crucial for managing dyslipidemia. Losing even a small amount of weight can significantly improve lipid levels and reduce the risk of heart disease.
Quitting Smoking
Smoking cessation is one of the most effective ways to improve lipid profiles and overall cardiovascular health. Quitting smoking can raise good cholesterol levels and reduce the risk of heart attacks and strokes.
Medications
In some cases, lifestyle changes alone may not be sufficient to manage dyslipidemia. Medications may be prescribed to help lower lipid levels and reduce the risk of complications.
Statins
Statins are the most commonly prescribed medications for lowering cholesterol levels. They work by inhibiting an enzyme in the liver that is responsible for producing cholesterol.
Fibrates
Fibrates are medications that primarily target triglyceride levels. They work by reducing the production of triglycerides in the liver and increasing the removal of triglycerides from the bloodstream.
Niacin
Niacin, also known as vitamin B3, can help lower triglyceride levels and raise good cholesterol levels. However, it is less commonly used due to potential side effects.
Bile Acid Sequestrants
These medications bind to bile acids in the intestines, preventing their reabsorption and prompting the liver to use cholesterol to produce more bile acids, thereby lowering cholesterol levels.
Ezetimibe
Ezetimibe works by reducing the absorption of cholesterol from the diet, leading to lower cholesterol levels in the blood.
Regular Monitoring
Regular follow-up appointments with a healthcare provider are essential for monitoring lipid levels and assessing the effectiveness of treatment. Adjustments to the treatment plan may be necessary based on the results of periodic lipid tests.
Complications of Untreated Dyslipidemia
If left untreated, dyslipidemia can lead to serious health complications, including:
- Coronary Artery Disease: Plaque buildup in the arteries that supply blood to the heart can lead to chest pain or heart attacks.
- Peripheral Artery Disease: Narrowed arteries in the legs can cause pain, cramping, and difficulty walking.
- Stroke: Plaque buildup in the arteries leading to the brain can result in a stroke.
- Pancreatitis: Extremely high triglyceride levels can cause inflammation of the pancreas, a condition known as pancreatitis.
Preventing Dyslipidemia
While some risk factors for dyslipidemia, such as genetics, cannot be changed, many preventive measures can be taken to reduce the risk of developing this condition.
Healthy Eating Habits
Adopting a balanced diet rich in fruits, vegetables, whole grains, and lean proteins can help maintain healthy lipid levels.
Regular Exercise
Engaging in regular physical activity not only helps manage weight but also improves lipid profiles and overall cardiovascular health.
Avoiding Tobacco and Excessive Alcohol
Quitting smoking and limiting alcohol consumption are important steps in preventing dyslipidemia and reducing the risk of heart disease.
Managing Underlying Health Conditions
Proper management of conditions such as diabetes, hypothyroidism, and obesity can help prevent dyslipidemia and its complications.