High calcium levels in the blood, also known as hypercalcemia, is a medical condition that occurs when there is an excessive amount of calcium circulating in the bloodstream. This imbalance can disrupt several bodily functions and lead to serious health complications if left untreated. While calcium is essential for maintaining strong bones, proper muscle function, and nerve signaling, too much of it can cause harm. Understanding the causes, recognizing the symptoms, and learning how to manage this condition are crucial steps in ensuring overall well-being.
What is Hypercalcemia?
Calcium is one of the most abundant minerals in the human body and plays a vital role in various physiological processes. It supports bone health, aids in blood clotting, regulates muscle contractions, and ensures proper nerve transmission. However, when the level of calcium in the blood exceeds the normal range, it leads to hypercalcemia. The normal range for calcium in the blood typically falls between 8.5 and 10.2 milligrams per deciliter. Anything above this range may indicate the presence of hypercalcemia.
Hypercalcemia can be mild or severe, depending on the underlying cause and the extent of the calcium elevation. Mild cases may not present noticeable symptoms, while severe cases can lead to life-threatening complications such as kidney damage or heart problems. Early detection and treatment are key to preventing long-term effects.
Causes of High Calcium Levels in the Blood
There are numerous potential causes of hypercalcemia, ranging from hormonal imbalances to certain medical conditions. Below are some of the most common factors that contribute to elevated calcium levels:
Overactive Parathyroid Glands
The parathyroid glands, located in the neck, are responsible for producing parathyroid hormone, which helps regulate calcium levels in the body. When these glands become overactive, they release excessive amounts of parathyroid hormone, leading to increased calcium absorption from the bones and intestines. This condition is known as hyperparathyroidism and is one of the leading causes of hypercalcemia.
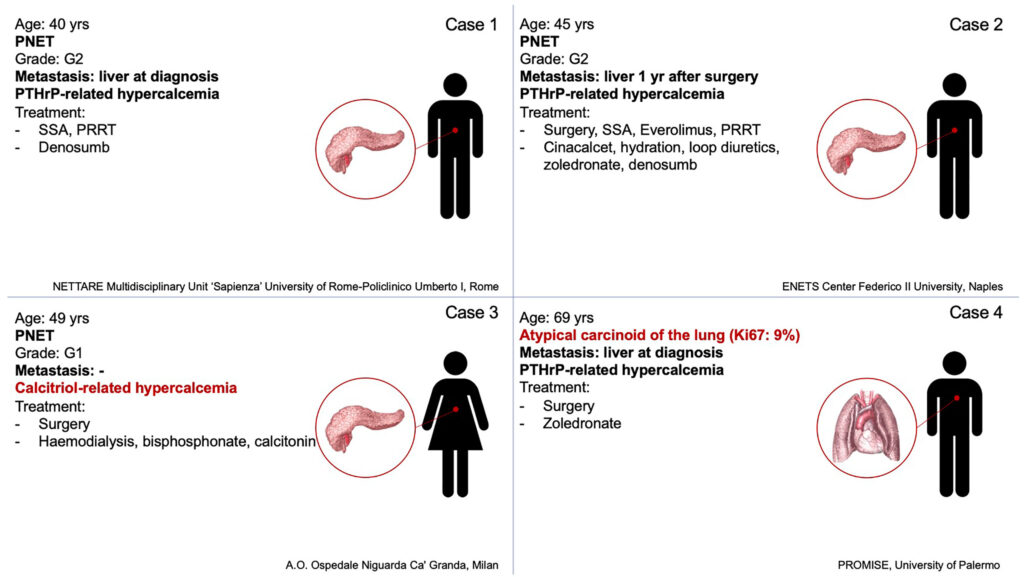
Cancer
Certain types of cancer, such as breast cancer, lung cancer, and multiple myeloma, can cause hypercalcemia. Cancer cells may produce substances that mimic parathyroid hormone, leading to increased calcium levels. Additionally, cancer can spread to the bones, causing them to release calcium into the bloodstream.
Vitamin D Disorders
Vitamin D plays a critical role in calcium absorption. Excessive intake of vitamin D supplements or conditions that cause the body to produce too much vitamin D can result in hypercalcemia. For example, sarcoidosis, a disease characterized by inflammation in the body, can lead to increased vitamin D production, which in turn raises calcium levels.
Medications
Some medications, particularly those used to treat osteoporosis or other bone-related conditions, can increase calcium levels. Examples include thiazide diuretics, which reduce the excretion of calcium in the urine, and lithium, which can affect parathyroid function.
Immobilization
Prolonged periods of inactivity, such as bed rest or immobilization due to injury, can lead to hypercalcemia. When bones are not subjected to regular stress or movement, they may begin to break down, releasing calcium into the bloodstream.
Other Causes
- Dehydration: Low fluid levels in the body can concentrate calcium in the blood, leading to elevated levels.
- Kidney Disorders: Impaired kidney function can interfere with the body’s ability to remove excess calcium through urine.
- Thyroid Problems: Overproduction of thyroid hormones can sometimes contribute to high calcium levels.
Symptoms of Hypercalcemia
The symptoms of hypercalcemia can vary depending on the severity of the condition and the individual’s overall health. In mild cases, there may be no noticeable symptoms at all. However, as calcium levels rise, the following signs and symptoms may develop:
Gastrointestinal Symptoms
- Nausea and vomiting
- Loss of appetite
- Constipation
- Abdominal pain
Kidney-Related Symptoms
- Frequent urination
- Excessive thirst
- Kidney stones, which can cause severe pain in the back or sides
Musculoskeletal Symptoms
- Muscle weakness
- Bone pain
- Fatigue
Neurological Symptoms
- Confusion or difficulty concentrating
- Depression
- Memory problems
- In severe cases, coma
Cardiovascular Symptoms
- Irregular heartbeat
- Hypertension (high blood pressure)
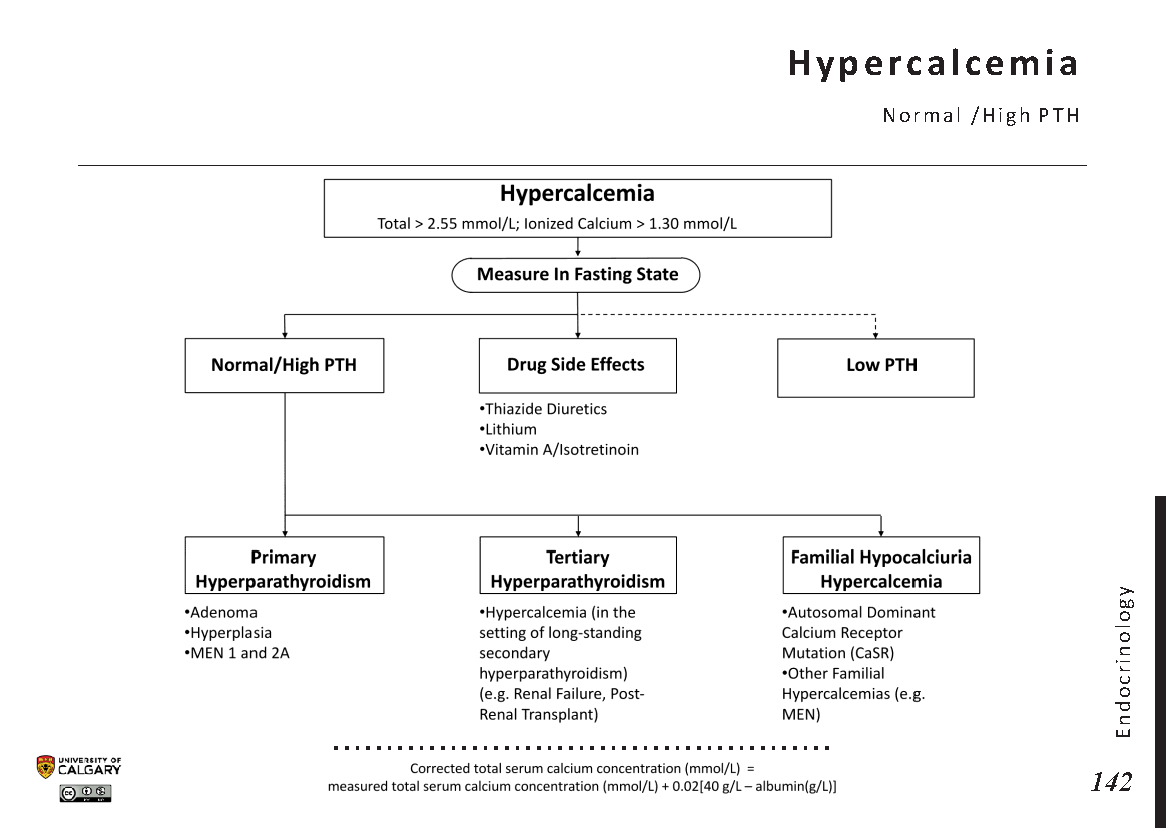
Diagnosis of Hypercalcemia
If hypercalcemia is suspected, healthcare providers will typically begin with a thorough medical history and physical examination. Blood tests are the primary diagnostic tool used to measure calcium levels in the blood. Additional tests may be ordered to determine the underlying cause of the condition. These may include:
- Parathyroid Hormone Test: Measures the level of parathyroid hormone in the blood to check for hyperparathyroidism.
- Vitamin D Test: Assesses whether vitamin D levels are contributing to the problem.
- Kidney Function Tests: Evaluates how well the kidneys are functioning.
- Imaging Studies: Such as X-rays, CT scans, or MRI scans, to identify any abnormalities in the bones or other organs.
Treatment Options for Hypercalcemia
The treatment for hypercalcemia depends on the underlying cause, the severity of the condition, and the patient’s overall health. The primary goal is to lower calcium levels in the blood and address the root cause of the problem. Below are some common treatment approaches:
Hydration
Intravenous fluids are often administered to help flush excess calcium from the body through the kidneys. This is especially important in cases where dehydration has contributed to elevated calcium levels.
Medications
- Bisphosphonates: These drugs help reduce bone breakdown and lower calcium levels in the blood. They are commonly used in cases of hypercalcemia caused by cancer.
- Calcitonin: A hormone that helps regulate calcium levels by decreasing bone resorption.
- Glucocorticoids: Steroids that can help reduce calcium levels in cases related to excessive vitamin D or sarcoidosis.
Dialysis
In severe cases where the kidneys are unable to remove excess calcium, dialysis may be necessary. This procedure helps filter waste and excess substances, including calcium, from the blood.
Surgery
If hyperparathyroidism is the cause of hypercalcemia, surgery to remove the overactive parathyroid gland(s) may be recommended. This procedure is known as a parathyroidectomy and is often curative.
Lifestyle Modifications
In addition to medical treatments, certain lifestyle changes can help manage hypercalcemia. These include:
- Reducing dietary calcium intake, particularly from dairy products and calcium supplements.
- Staying well-hydrated by drinking plenty of water.
- Avoiding excessive sun exposure, which can increase vitamin D production.
Preventing Hypercalcemia
While not all cases of hypercalcemia can be prevented, there are steps individuals can take to reduce their risk. Regular check-ups with a healthcare provider can help monitor calcium levels, especially for those with a family history of parathyroid disorders or other risk factors. Additionally, avoiding excessive use of calcium or vitamin D supplements without medical supervision is crucial.
Living with Hypercalcemia
Managing hypercalcemia requires ongoing care and attention. Patients should work closely with their healthcare team to monitor their condition and adjust treatment plans as needed. Education about the condition and its potential complications is also important for making informed decisions about care.
Support groups and counseling may be beneficial for individuals dealing with the emotional and psychological impact of chronic health conditions. By staying proactive and informed, patients can better manage their symptoms and improve their quality of life.