A hiatal hernia, often abbreviated as HH, is a condition where part of the stomach pushes upward through an opening in the diaphragm called the hiatus. This can lead to various symptoms and complications, depending on the type and severity of the hernia. Understanding this condition is essential for early detection, proper management, and effective treatment. In this article, we will explore the different aspects of hiatal hernia, including its types, symptoms, diagnosis, and treatment options.
Overview of Hiatal Hernia
The diaphragm is a large muscle that separates the chest cavity from the abdominal cavity. It plays a crucial role in breathing and also helps keep the stomach in place below it. The hiatus is a natural opening in the diaphragm that allows the esophagus to pass through and connect to the stomach. When a portion of the stomach protrudes through this opening, it results in a hiatal hernia.
This condition is more common in individuals over the age of 50 and tends to affect women more frequently than men. While some people may not experience any symptoms, others may suffer from discomfort or complications such as gastroesophageal reflux disease.
Causes of Hiatal Hernia
- Weakened Muscles: The muscles around the hiatus may weaken due to aging, injury, or congenital factors, allowing the stomach to push through.
- Injury: Trauma to the area, such as from surgery or an accident, can contribute to the development of a hiatal hernia.
- Persistent Pressure: Activities that put pressure on the abdomen, such as heavy lifting, persistent coughing, or straining during bowel movements, can increase the risk.
- Obesity: Excess weight can put additional pressure on the abdomen, increasing the likelihood of developing this condition.
Types of Hiatal Hernia
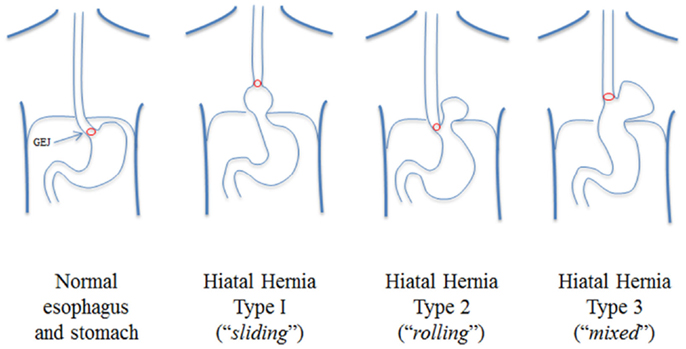
There are two primary types of hiatal hernia, each with distinct characteristics and implications.
Type 1: Sliding Hiatal Hernia
This is the most common type of hiatal hernia, accounting for the majority of cases. In a sliding hiatal hernia, the upper part of the stomach and the junction where the esophagus meets the stomach slide up into the chest through the hiatus. This type is often associated with gastroesophageal reflux disease because the displacement can disrupt the normal function of the lower esophageal sphincter, leading to acid reflux.
Type 2: Paraesophageal Hiatal Hernia
A paraesophageal hiatal hernia occurs when part of the stomach squeezes through the hiatus and positions itself next to the esophagus. Unlike the sliding type, the junction between the esophagus and stomach remains in its normal location. While less common, this type can be more serious because there is a risk of the herniated portion of the stomach becoming trapped or having its blood supply cut off, leading to complications like strangulation.
Symptoms of Hiatal Hernia
Many people with a hiatal hernia do not experience noticeable symptoms. However, when symptoms do occur, they can range from mild to severe and may include:
- Chest Pain: A burning sensation or discomfort in the chest, often mistaken for heart-related pain.
- Heartburn: A common symptom caused by acid reflux, characterized by a burning feeling in the chest or throat.
- Difficulty Swallowing: Also known as dysphagia, this occurs when the hernia affects the passage of food through the esophagus.
- Regurgitation: The backflow of stomach contents, including acid, into the mouth.
- Bloating: A feeling of fullness or swelling in the abdomen.
- Hiccups: Persistent hiccups can sometimes be linked to a hiatal hernia.
When to Seek Medical Attention
If you experience severe chest pain, difficulty swallowing, or vomiting blood, it is important to seek medical attention immediately. These symptoms could indicate complications such as strangulation or bleeding, which require prompt treatment.
Diagnosis of Hiatal Hernia
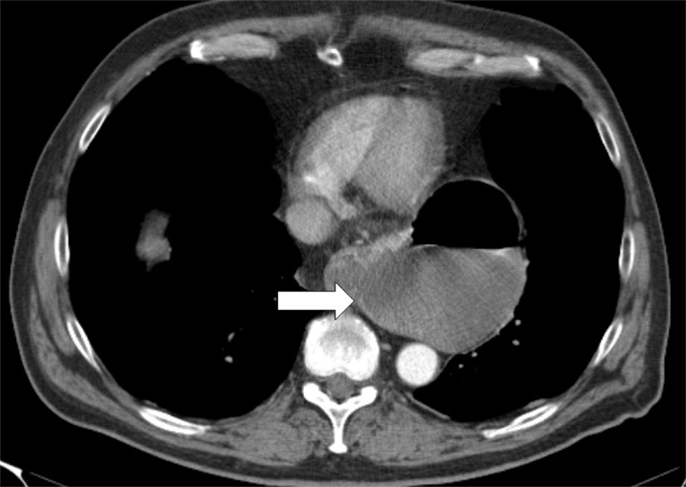
Diagnosing a hiatal hernia typically involves a combination of physical examinations and diagnostic tests. Since many cases are asymptomatic, the condition is often discovered incidentally during tests for other conditions.
Physical Examination
A healthcare provider may begin by asking about your symptoms and medical history. They might also perform a physical examination, although a hiatal hernia cannot usually be felt during a routine check-up.
Diagnostic Tests
- X-ray with Barium Swallow: You will drink a liquid containing barium, which coats the digestive tract and makes it visible on an X-ray. This test helps identify abnormalities in the esophagus and stomach.
- Endoscopy: A thin, flexible tube with a camera is inserted through the mouth to examine the esophagus and stomach. This procedure can help detect inflammation, ulcers, or other issues related to the hernia.
- Esophageal Manometry: This test measures the strength and coordination of the esophageal muscles, helping to assess how well the esophagus is functioning.
- pH Monitoring: A small device is placed in the esophagus to measure acid levels over a 24-hour period, helping to diagnose acid reflux associated with a hiatal hernia.
Treatment Options for Hiatal Hernia
Treatment for a hiatal hernia depends on the type, severity, and symptoms experienced by the individual. In many cases, lifestyle changes and medications are sufficient to manage the condition, while surgery may be necessary for more severe cases.
Lifestyle Modifications
Making certain adjustments to your daily habits can significantly reduce symptoms and prevent complications:
- Dietary Changes: Avoid foods that trigger acid reflux, such as spicy, fatty, or acidic foods. Eating smaller, more frequent meals can also help.
- Elevating the Head of the Bed: Raising the head of your bed by a few inches can reduce nighttime acid reflux.
- Avoiding Lying Down After Meals: Wait at least two to three hours after eating before lying down or going to bed.
- Weight Management: Losing excess weight can alleviate pressure on the abdomen and reduce symptoms.
- Quitting Smoking: Smoking can weaken the lower esophageal sphincter and worsen acid reflux.
Medications
Several medications can help manage symptoms and reduce acid production:
- Antacids: Over-the-counter medications that neutralize stomach acid and provide quick relief.
- H2 Blockers: These medications reduce acid production and are available both over-the-counter and by prescription.
- Proton Pump Inhibitors: Stronger medications that block acid production and allow the esophagus to heal.
Surgical Intervention
Surgery is typically reserved for cases where lifestyle changes and medications fail to provide relief, or when complications arise. The most common surgical procedure for a hiatal hernia is called fundoplication. During this procedure, the surgeon wraps the upper part of the stomach around the lower esophagus to strengthen the lower esophageal sphincter and prevent acid reflux.
In some cases, minimally invasive techniques such as laparoscopic surgery may be used, resulting in faster recovery times and less postoperative pain. However, surgery carries risks and should only be considered after thorough evaluation and discussion with a healthcare provider.
Risks and Considerations
While surgery can effectively treat a hiatal hernia, it is not without risks. Potential complications include infection, bleeding, and recurrence of the hernia. It is important to weigh the benefits against the risks and discuss all available options with your doctor.
Living with a Hiatal Hernia
For many individuals, living with a hiatal hernia involves managing symptoms through lifestyle changes and medication. Regular follow-ups with a healthcare provider are essential to monitor the condition and make adjustments to the treatment plan as needed.
Education and awareness play a key role in managing this condition. By understanding the triggers and taking proactive steps, individuals can minimize discomfort and improve their quality of life.