Herpangina, often abbreviated as HA, is a common yet uncomfortable condition that primarily affects children. It is characterized by small ulcers or sores in the mouth, which can cause significant discomfort and pain. This guide aims to provide comprehensive information about this condition, including its causes, symptoms, diagnosis, treatment options, and prevention strategies.
What is Herpangina?
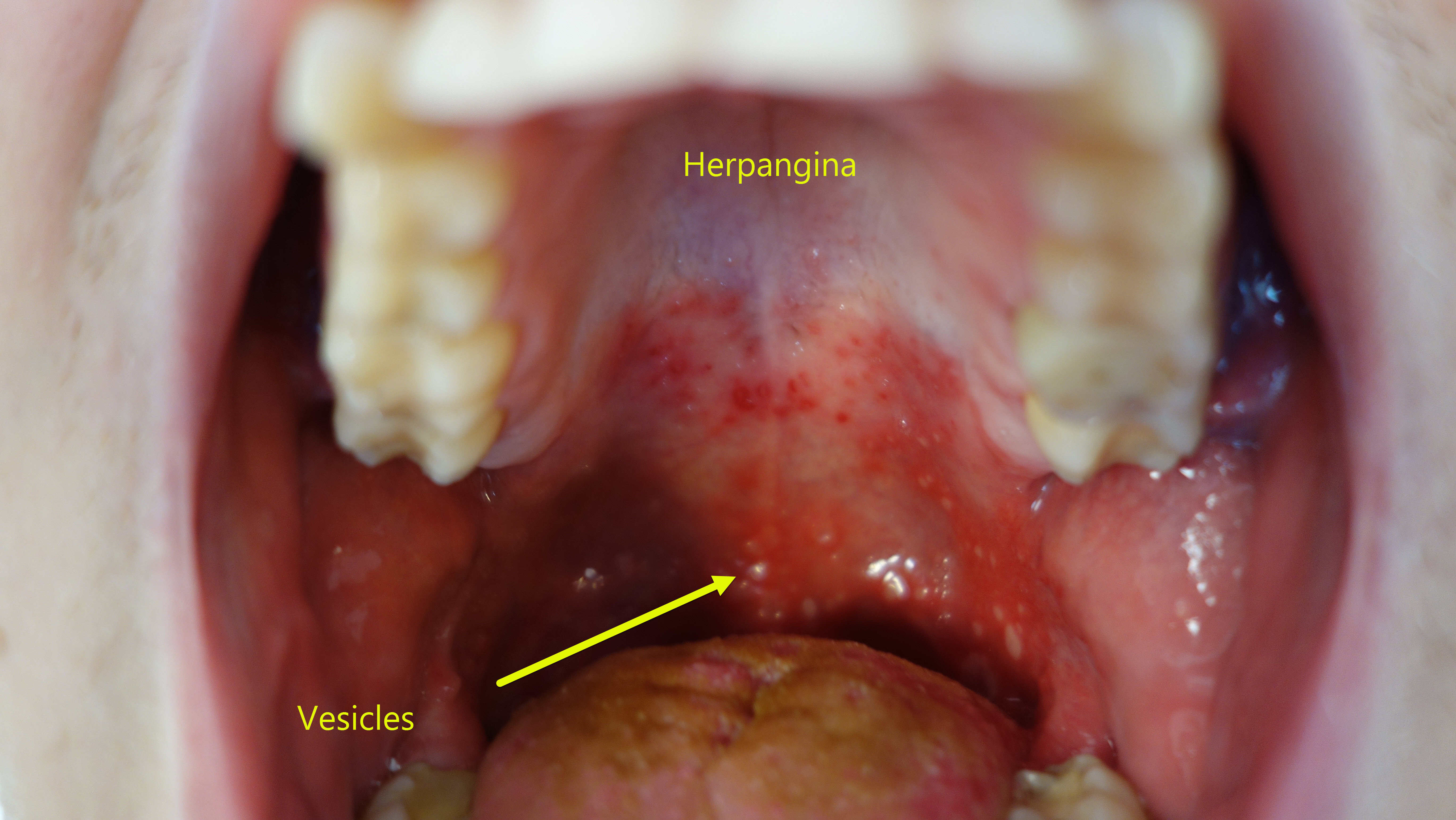
Herpangina is a viral infection that leads to the formation of painful sores or ulcers in the mouth, particularly at the back of the throat. The condition is most commonly seen in children aged three to ten years but can also affect adults, though less frequently. The name “herpangina” might suggest a connection to herpes, but it is unrelated to the herpes simplex virus. Instead, herpangina is caused by a group of viruses known as enteroviruses.
Causes of Herpangina
The primary cause of herpangina is an infection by certain types of enteroviruses. These viruses are highly contagious and spread through direct contact with an infected person or contaminated surfaces. Below are some of the main factors contributing to the spread of herpangina:
- Contact with Infected Individuals: Close contact, such as hugging, kissing, or sharing utensils, can transmit the virus.
- Contaminated Surfaces: Touching objects like toys, doorknobs, or countertops that have been touched by an infected person can lead to transmission.
- Poor Hygiene Practices: Not washing hands regularly or thoroughly can increase the risk of contracting the virus.
- Crowded Environments: Schools, daycare centers, and summer camps are common places where outbreaks occur due to close proximity among children.
Symptoms of Herpangina
The symptoms of herpangina typically appear within three to six days after exposure to the virus. While the severity of symptoms may vary, they generally include:
- Fever: A sudden high fever is often one of the first signs of herpangina.
- Sore Throat: Children may complain of a severe sore throat, making it difficult to swallow.
- Mouth Ulcers: Small, grayish-white ulcers with red borders usually develop on the roof of the mouth, tonsils, or the back of the throat.
- Loss of Appetite: Pain from the ulcers can lead to a decreased desire to eat or drink.
- Vomiting: Some children may experience nausea or vomiting.
- Headache: Mild to moderate headaches are also common during the course of the illness.
How is Herpangina Diagnosed?
Diagnosing herpangina involves a combination of physical examination and patient history. Since the symptoms of herpangina are similar to those of other viral infections, healthcare providers rely on specific indicators to confirm the diagnosis:
- Physical Examination: The doctor will examine the mouth and throat for characteristic ulcers and assess other symptoms like fever and sore throat.
- Medical History: Information about recent exposure to sick individuals or attendance at crowded places helps in identifying potential sources of infection.
- Laboratory Tests: In rare cases, throat swabs or stool samples may be collected to identify the specific virus causing the infection.
Treatment Options for Herpangina
There is no specific antiviral medication available to treat herpangina, as it is a self-limiting condition that resolves on its own within seven to ten days. However, several measures can help alleviate symptoms and ensure comfort during recovery:
Pain Relief
- Over-the-Counter Pain Relievers: Acetaminophen or ibuprofen can be used to reduce fever and relieve pain. Always consult a healthcare provider before administering any medication to children.
- Topical Anesthetics: Gels or sprays containing numbing agents can be applied directly to the ulcers to provide temporary relief.
Hydration
- Encourage Fluid Intake: Staying hydrated is crucial, especially since swallowing may be painful. Offer cool water, ice chips, or popsicles to soothe the throat.
- Avoid Acidic or Spicy Foods: These can irritate the ulcers further and should be avoided until the condition improves.
Rest and Comfort
- Adequate Rest: Ensure the child gets plenty of rest to support the immune system in fighting off the infection.
- Humidifier Use: Using a cool-mist humidifier can ease breathing and reduce throat irritation.
Prevention Strategies for Herpangina
While it may not always be possible to prevent herpangina, adopting good hygiene practices can significantly reduce the risk of infection:
- Regular Handwashing: Teach children to wash their hands frequently with soap and water, especially before meals and after using the restroom.
- Avoid Sharing Personal Items: Discourage sharing of cups, utensils, towels, or toys with others, particularly in group settings.
- Clean and Disinfect Surfaces: Regularly clean and disinfect commonly touched surfaces to minimize the spread of germs.
- Stay Home When Sick: Keep children home from school or daycare if they exhibit symptoms of herpangina to prevent spreading the virus to others.
When to Seek Medical Attention
While herpangina is generally mild and resolves without complications, there are situations where medical attention is necessary:
- Persistent High Fever: If the fever does not subside after a few days or exceeds 103 degrees Fahrenheit, seek medical advice.
- Dehydration Signs: Symptoms such as dry mouth, reduced urine output, or extreme lethargy could indicate dehydration, requiring immediate care.
- Severe Pain: If the pain becomes unbearable despite over-the-counter remedies, consult a healthcare provider for alternative solutions.
- Worsening Symptoms: Any worsening of symptoms or development of new ones should prompt a visit to the doctor.
Understanding the Difference Between Herpangina and Other Conditions
Herpangina shares similarities with other illnesses, such as hand-foot-and-mouth disease and strep throat. Understanding the differences can aid in accurate diagnosis and appropriate treatment:
- Hand-Foot-and-Mouth Disease: Unlike herpangina, this condition causes rashes on the hands and feet in addition to mouth ulcers.
- Strep Throat: Strep throat is caused by bacteria rather than a virus and requires antibiotic treatment. It does not involve mouth ulcers.
By being aware of these distinctions, parents and caregivers can better navigate the healthcare system and ensure proper management of the child’s condition.





