A herniated disc, often referred to as a slipped disc or ruptured disc, is a common spinal condition that can cause significant discomfort and limit mobility. This condition occurs when the soft, gel-like center of a spinal disc pushes through a crack in the tougher exterior casing. While the term “slipped disc” is widely used, it is important to note that the disc does not actually slip out of place but rather bulges or ruptures. In this article, we will explore the causes, symptoms, and available treatments for this condition.
Understanding the Spine and Discs
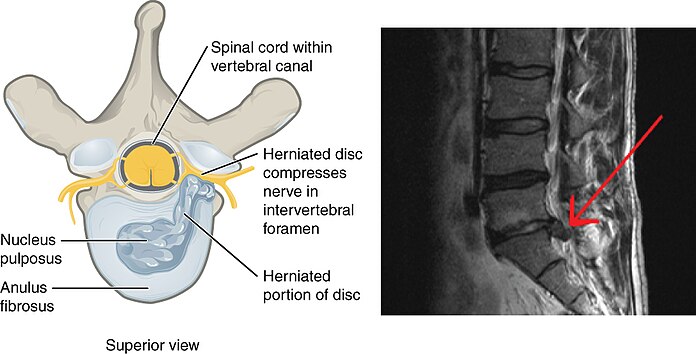
The spine is made up of a series of bones called vertebrae, which are separated by intervertebral discs. These discs act as cushions, absorbing shock and allowing flexibility in the spine. Each disc has two main components: the annulus fibrosus, which is the tough outer layer, and the nucleus pulposus, which is the soft inner core. When a disc becomes herniated, the nucleus pulposus leaks out through a tear in the annulus fibrosus, potentially pressing on nearby nerves and causing pain or other symptoms.
How Common Is a Herniated Disc?
Herniated discs are a prevalent issue, particularly among adults aged 30 to 50. They are more common in men than women and often occur in the lower back, although they can also affect the neck. Despite their frequency, many people with herniated discs do not experience noticeable symptoms and may never require treatment.
Causes of a Herniated Disc
Several factors can contribute to the development of a herniated disc. Understanding these causes can help individuals take preventive measures and reduce their risk of experiencing this condition.
Age-Related Wear and Tear
As people age, the discs in the spine naturally lose water content, making them less flexible and more prone to tearing or rupturing. This process, known as disc degeneration, is a leading cause of herniated discs. Even minor strains or twists can lead to a herniation in older adults.
Injury or Trauma
Sudden injuries, such as those sustained in car accidents or falls, can cause the outer layer of a disc to tear, leading to herniation. Additionally, repetitive strain from activities like heavy lifting or improper body mechanics can weaken the discs over time, increasing the likelihood of rupture.
Lifestyle Factors
- Obesity: Excess body weight places additional stress on the spine, particularly the lower back, increasing the risk of disc herniation.
- Sedentary Lifestyle: Lack of physical activity can weaken the muscles that support the spine, making it more vulnerable to injury.
- Poor Posture: Slouching or maintaining improper posture for extended periods can strain the spine and contribute to disc problems.
Symptoms of a Herniated Disc
The symptoms of a herniated disc vary depending on its location and severity. Some individuals may experience no symptoms at all, while others may face debilitating pain or neurological issues.
Common Symptoms
- Localized Pain: A herniated disc in the lower back may cause pain in the lower back itself, while one in the neck may lead to neck pain.
- Radiating Pain: The most common symptom is pain that radiates along the path of a compressed nerve. For example, a herniated disc in the lower back can cause sciatica, characterized by sharp, shooting pain down the leg.
- Numbness or Tingling: Individuals may experience numbness or a tingling sensation in the area served by the affected nerve.
- Muscle Weakness: Nerve compression can weaken the muscles controlled by that nerve, leading to difficulty lifting objects, walking, or performing daily tasks.
When to Seek Medical Attention
While mild cases of herniated discs may resolve on their own, certain symptoms warrant immediate medical attention. These include:
- Severe or worsening pain that does not improve with rest
- Loss of bladder or bowel control, which could indicate cauda equina syndrome
- Progressive weakness in the limbs
Diagnosing a Herniated Disc
Diagnosing a herniated disc typically involves a combination of physical examination and imaging tests. A healthcare provider will assess the patient’s symptoms, medical history, and perform specific maneuvers to check for nerve irritation or compression.
Imaging Tests
- Magnetic Resonance Imaging (MRI): This test provides detailed images of the spine and is the most effective way to identify a herniated disc.
- X-rays: While X-rays cannot detect herniated discs, they can rule out other conditions, such as fractures or tumors.
- Computed Tomography (CT) Scan: A CT scan may be used to provide cross-sectional images of the spine.
- Electromyography (EMG): This test measures electrical activity in the muscles and can help determine if a herniated disc is affecting nerve function.
Treatment Options for a Herniated Disc
Treatment for a herniated disc depends on the severity of symptoms and the impact on daily life. Many cases can be managed with conservative, non-surgical approaches, while others may require more advanced interventions.
Conservative Treatments
Non-surgical treatments are often the first line of defense against a herniated disc. These methods aim to relieve pain, reduce inflammation, and promote healing.
Rest and Activity Modification
Short periods of rest can help alleviate acute pain, but prolonged bed rest is generally discouraged, as it may weaken the muscles supporting the spine. Instead, individuals are encouraged to modify their activities to avoid movements that exacerbate symptoms.
Physical Therapy
Physical therapy plays a crucial role in managing herniated discs. A therapist can design a personalized exercise program to strengthen the core and back muscles, improve flexibility, and correct posture. Specific stretches and exercises can also help relieve pressure on the affected nerve.
Medications
Over-the-counter pain relievers, such as ibuprofen or acetaminophen, are often recommended to manage mild to moderate pain. For more severe cases, a doctor may prescribe stronger medications, including muscle relaxants, nerve pain medications, or corticosteroids to reduce inflammation.
Epidural Steroid Injections
In cases where pain persists despite other treatments, an epidural steroid injection may be considered. This procedure involves injecting a corticosteroid medication directly into the space around the affected nerve to reduce inflammation and alleviate pain.
Surgical Treatments
If conservative treatments fail to provide relief after several weeks or months, surgery may be necessary. Surgical options are typically reserved for severe cases involving significant nerve damage or loss of function.
Microdiscectomy
This minimally invasive procedure involves removing the portion of the disc that is pressing on the nerve. It is one of the most common surgeries performed for herniated discs and often results in rapid pain relief.
Spinal Fusion
In rare cases, a spinal fusion may be recommended to stabilize the spine. This procedure involves joining two or more vertebrae together to prevent movement that could cause pain.
Artificial Disc Replacement
For some patients, replacing the damaged disc with an artificial one may be an option. This procedure aims to preserve spinal mobility while alleviating symptoms.
Preventing a Herniated Disc
While not all cases of herniated discs can be prevented, certain lifestyle changes can significantly reduce the risk of developing this condition.
Maintain a Healthy Weight
Excess weight places additional strain on the spine, so maintaining a healthy weight through a balanced diet and regular exercise is essential.
Practice Proper Lifting Techniques
When lifting heavy objects, use your legs rather than your back to avoid straining the spine. Keep the object close to your body and avoid twisting while lifting.
Exercise Regularly
Engaging in regular physical activity strengthens the muscles supporting the spine and improves overall flexibility. Focus on exercises that target the core and back muscles, such as yoga, Pilates, or swimming.
Adopt Good Posture
Whether sitting, standing, or sleeping, maintaining proper posture helps reduce stress on the spine. Use ergonomic furniture and supportive pillows to encourage good alignment.
Living with a Herniated Disc
Managing a herniated disc requires patience and persistence. While the condition can be painful and disruptive, many individuals find relief through a combination of treatments and lifestyle adjustments. By staying informed and working closely with healthcare providers, patients can take proactive steps toward recovery and improved quality of life.