Hemophilia, often abbreviated as Hemo, is a rare genetic disorder that affects the body’s ability to form blood clots. This condition primarily arises due to deficiencies in specific clotting factors, with Factor Eight being one of the most commonly affected. People living with this condition face challenges such as prolonged bleeding after injuries, spontaneous bleeding episodes, and an increased risk of joint damage. In this article, we will explore the causes, symptoms, diagnosis, treatment, and management of this condition to provide a comprehensive understanding of this bleeding disorder.
What is Hemophilia?
Hemophilia is a hereditary bleeding disorder characterized by the inability of blood to clot properly. This happens because the body lacks sufficient levels of certain proteins, known as clotting factors, which are essential for stopping bleeding. The two main types of hemophilia are classified based on the specific clotting factor that is deficient. The type associated with Factor Eight deficiency is the most common and is referred to as Hemophilia A. Another type, caused by a deficiency in Factor Nine, is called Hemophilia B.
The severity of hemophilia varies depending on the level of clotting factor activity in the blood. Individuals with mild cases may experience bleeding only after significant trauma or surgery, while those with severe forms may suffer from spontaneous bleeding without any apparent cause.
How Blood Clotting Works
To understand hemophilia, it is important to first grasp how the normal blood clotting process works. When a blood vessel is injured, the body initiates a series of steps to stop the bleeding:
- Vasoconstriction: The blood vessel narrows to reduce blood flow to the injured area.
- Platelet Plug Formation: Platelets, small cell fragments in the blood, gather at the injury site and stick together to form a temporary plug.
- Clotting Cascade: A complex chain reaction involving clotting factors activates fibrin, a protein that reinforces the platelet plug and forms a stable clot.
In individuals with hemophilia, the clotting cascade is disrupted due to insufficient levels of specific clotting factors, leading to prolonged bleeding.
Causes of Hemophilia
Hemophilia is primarily a genetic disorder caused by mutations in genes responsible for producing clotting factors. These genes are located on the X chromosome, making hemophilia an X-linked recessive condition. This means that the disorder predominantly affects males, while females are typically carriers who may pass the gene to their offspring.
In rare cases, hemophilia can occur due to spontaneous mutations, even if there is no family history of the disorder. This happens when a new genetic change occurs during the formation of reproductive cells or early fetal development.
Inheritance Patterns
The inheritance pattern of hemophilia depends on whether the mother is a carrier or if the father has the disorder:
- If a mother is a carrier and the father does not have hemophilia, each son has a fifty percent chance of inheriting the condition, while each daughter has a fifty percent chance of being a carrier.
- If a father has hemophilia and the mother does not carry the gene, none of the sons will inherit the disorder, but all daughters will be carriers.
Symptoms of Hemophilia
The symptoms of hemophilia vary based on the severity of the clotting factor deficiency. Common signs and symptoms include:
- Prolonged bleeding after cuts, injuries, or surgeries
- Large or deep bruises that appear without a clear cause
- Unexplained nosebleeds that are difficult to stop
- Bleeding into joints, leading to swelling, pain, and stiffness
- Blood in urine or stool
- Spontaneous bleeding in muscles or soft tissues
In severe cases, internal bleeding can occur in critical areas such as the brain, which may result in life-threatening complications.
Bleeding into Joints
One of the hallmark symptoms of hemophilia is bleeding into joints, also known as hemarthrosis. This occurs when blood accumulates in the joint space, causing pain, swelling, and reduced mobility. Repeated episodes of joint bleeding can lead to long-term damage, including arthritis and joint deformities.
Diagnosing Hemophilia
Diagnosing hemophilia involves a combination of clinical evaluation, family history assessment, and laboratory tests. If a healthcare provider suspects hemophilia based on symptoms or family history, they will order specific blood tests to confirm the diagnosis.
Blood Tests for Hemophilia
The primary diagnostic tests for hemophilia include:
- Complete Blood Count: This test measures the levels of red blood cells, white blood cells, and platelets in the blood.
- Prothrombin Time: This test evaluates the extrinsic pathway of the clotting cascade and helps rule out other bleeding disorders.
- Activated Partial Thromboplastin Time: This test assesses the intrinsic pathway of the clotting cascade and is often prolonged in individuals with hemophilia.
- Factor Activity Assay: This specialized test measures the activity levels of specific clotting factors, such as Factor Eight or Factor Nine, to determine the type and severity of hemophilia.
Treatment Options for Hemophilia
While there is no cure for hemophilia, several treatment options are available to manage the condition and prevent complications. The goal of treatment is to replace the missing clotting factor and control bleeding episodes effectively.
Clotting Factor Replacement Therapy
Clotting factor replacement therapy is the cornerstone of hemophilia treatment. This involves infusing concentrated clotting factor into the bloodstream to restore normal clotting function. There are two main types of clotting factor products:
- Plasma-Derived Factors: These are extracted from human blood plasma and purified for use.
- Recombinant Factors: These are produced using genetically engineered cells and do not involve human blood products, reducing the risk of infections.
Replacement therapy can be administered on-demand to treat acute bleeding episodes or as prophylaxis to prevent bleeding in individuals with severe hemophilia.
Desmopressin Acetate
For individuals with mild hemophilia, a synthetic hormone called desmopressin acetate may be used to stimulate the release of stored clotting factors. This medication is administered through injection or nasal spray and is effective for managing minor bleeding episodes.
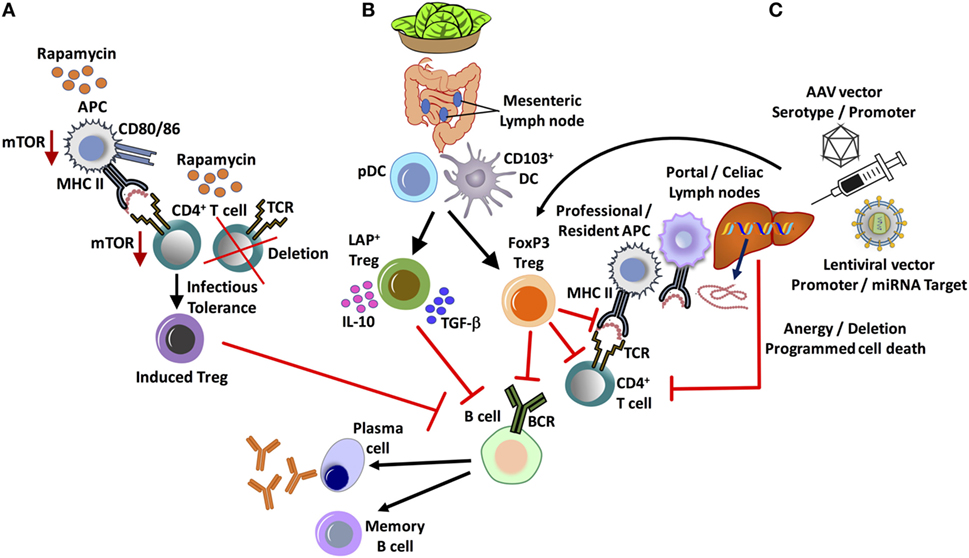
Gene Therapy
Recent advancements in medical research have led to the development of gene therapy as a potential treatment for hemophilia. This innovative approach involves introducing a functional copy of the defective gene into the patient’s cells, enabling the body to produce the missing clotting factor naturally. While still in the experimental stages, gene therapy holds promise for providing long-term relief from the condition.
Managing Hemophilia in Daily Life
Living with hemophilia requires careful planning and proactive management to minimize the risk of bleeding episodes and maintain overall health. Here are some key strategies for managing the condition:
Avoiding Injury
Individuals with hemophilia should take precautions to avoid injuries that could lead to bleeding. This includes wearing protective gear during physical activities, avoiding contact sports, and ensuring a safe home environment.
Regular Medical Check-Ups
Frequent visits to a hematologist or specialist are essential for monitoring the condition and adjusting treatment plans as needed. Regular check-ups also help detect and address complications such as joint damage or inhibitor development early.
Educating Family and Caregivers
Family members and caregivers play a crucial role in supporting individuals with hemophilia. Educating them about the condition, recognizing signs of bleeding, and knowing how to administer first aid can make a significant difference in managing emergencies.
Complications Associated with Hemophilia
Despite advances in treatment, individuals with hemophilia may experience complications that impact their quality of life. Some of the most common complications include:
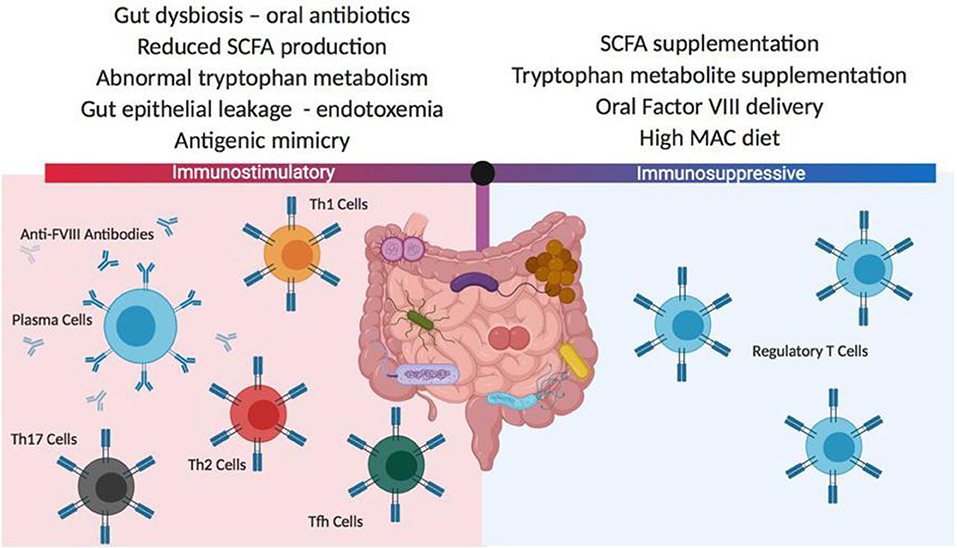
- Development of inhibitors, which are antibodies that attack infused clotting factors and reduce their effectiveness
- Chronic joint damage and arthritis due to repeated bleeding into joints
- Infections transmitted through contaminated blood products (though this risk has significantly decreased with modern screening techniques)
- Life-threatening bleeding in vital organs such as the brain or gastrointestinal tract
Addressing Inhibitors
Inhibitors are a serious complication that occurs when the immune system mistakenly targets infused clotting factors. Managing inhibitors often requires specialized treatments, such as immune tolerance induction therapy or bypassing agents, to control bleeding effectively.