Heart failure, often abbreviated as HF, is a serious medical condition that affects millions of people worldwide. It occurs when the heart is unable to pump blood effectively, leading to a range of symptoms and complications. This article delves into the intricacies of heart failure, exploring its causes, risk factors, symptoms, and available management strategies. By understanding this condition, individuals can take proactive steps to improve their health outcomes.
What is Heart Failure?
Heart failure is not a single disease but rather a syndrome that arises from various underlying conditions affecting the heart’s ability to function properly. When the heart cannot pump enough blood to meet the body’s needs, it leads to a cascade of problems, including fluid buildup, fatigue, and shortness of breath. This condition can develop suddenly or progress over time, depending on its cause and severity.
Types of Heart Failure
- Left-sided heart failure: This occurs when the left ventricle, the heart’s main pumping chamber, cannot effectively pump oxygen-rich blood to the rest of the body. It is further categorized into two types:
- Systolic heart failure: The heart muscle weakens and cannot contract forcefully enough to pump blood out.
- Diastolic heart failure: The heart muscle becomes stiff and cannot relax properly, preventing it from filling with enough blood between beats.
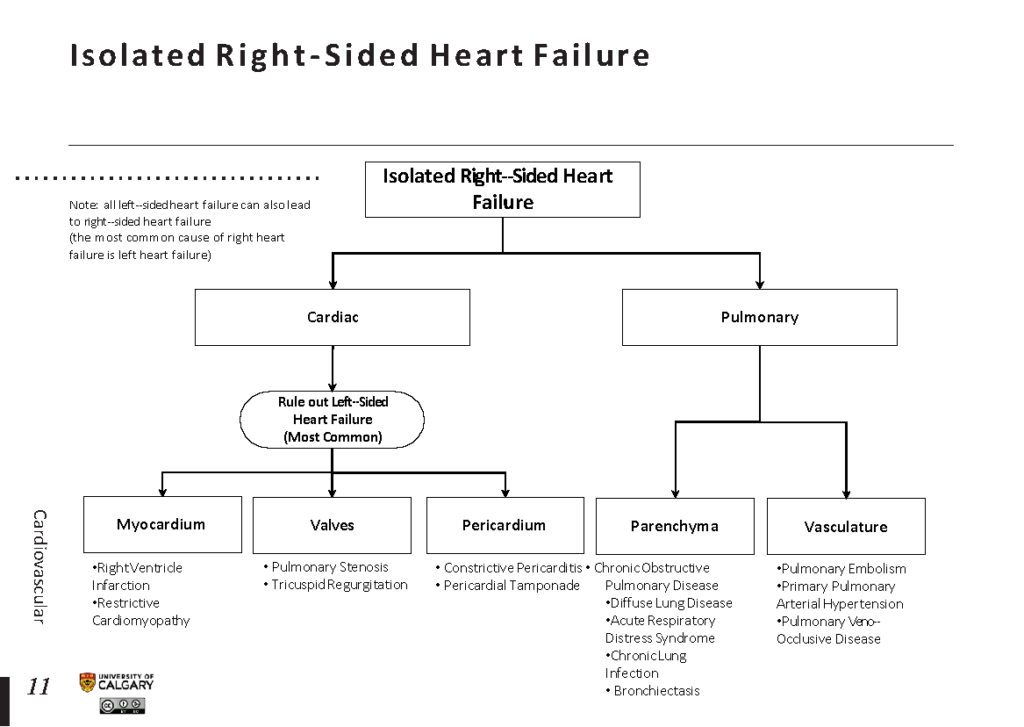
- Right-sided heart failure: This happens when the right ventricle struggles to pump blood to the lungs for oxygenation. It often results from left-sided heart failure, as the increased pressure in the lungs strains the right side of the heart.
- Congestive heart failure: A term used when fluid builds up around the heart and in other parts of the body, such as the lungs, legs, and abdomen.
Causes of Heart Failure
Heart failure can result from a variety of conditions that damage or weaken the heart. Some of the most common causes include:
Coronary Artery Disease
Coronary artery disease occurs when the arteries supplying blood to the heart become narrowed or blocked due to plaque buildup. This reduces blood flow to the heart muscle, leading to damage and weakening over time. Heart attacks, which are caused by sudden blockages in these arteries, can also severely impair heart function.
High Blood Pressure
When blood pressure remains consistently high, the heart must work harder to pump blood throughout the body. Over time, this extra strain can cause the heart muscle to thicken and become less efficient, eventually leading to heart failure.
Cardiomyopathy
Cardiomyopathy refers to diseases of the heart muscle, which can be inherited or acquired. These conditions cause the heart muscle to become enlarged, thickened, or rigid, impairing its ability to pump blood effectively.
Heart Valve Disorders
The heart contains four valves that ensure blood flows in the correct direction. If these valves become damaged or diseased, they may not open or close properly, forcing the heart to work harder and potentially leading to heart failure.
Other Contributing Factors
- Arrhythmias: Irregular heartbeats, such as atrial fibrillation, can disrupt the heart’s pumping efficiency.
- Diabetes: Poorly controlled diabetes increases the risk of coronary artery disease and high blood pressure, both of which contribute to heart failure.
- Obesity: Excess weight places additional strain on the heart and is linked to other risk factors like high blood pressure and diabetes.
- Chronic Kidney Disease: Impaired kidney function can lead to fluid retention and high blood pressure, further taxing the heart.
Symptoms of Heart Failure
The symptoms of heart failure vary depending on its severity and the specific areas of the body affected. Common signs include:
- Shortness of breath: This may occur during physical activity, at rest, or while lying down.
- Fatigue and weakness: Reduced blood flow to muscles and tissues can leave individuals feeling constantly tired.
- Swelling: Fluid retention can cause swelling in the legs, ankles, feet, or abdomen.
- Rapid or irregular heartbeat: The heart may beat faster or irregularly as it tries to compensate for reduced pumping efficiency.
- Persistent coughing or wheezing: Fluid buildup in the lungs can lead to these respiratory symptoms.
- Reduced ability to exercise: Individuals may find it increasingly difficult to perform physical activities.
Diagnosing Heart Failure
Diagnosing heart failure involves a combination of medical history evaluation, physical examinations, and diagnostic tests. Healthcare providers look for signs such as abnormal heart sounds, fluid retention, and elevated jugular vein pressure. Key diagnostic tools include:
Echocardiogram
An echocardiogram uses sound waves to create images of the heart, allowing doctors to assess its structure and function. This test helps determine the ejection fraction, or the percentage of blood pumped out of the heart with each contraction.
Electrocardiogram (ECG)
An electrocardiogram records the electrical activity of the heart, identifying abnormalities in rhythm or evidence of previous heart attacks.
Blood Tests
Blood tests can detect markers of heart failure, such as elevated levels of B-type natriuretic peptide, which is released by the heart in response to stress.
Chest X-ray
A chest X-ray can reveal an enlarged heart or fluid accumulation in the lungs, both of which are indicative of heart failure.
Managing Heart Failure
While heart failure is a chronic condition, proper management can significantly improve quality of life and reduce the risk of complications. Treatment plans are tailored to the individual and typically involve a combination of lifestyle changes, medications, and, in some cases, surgical interventions.
Lifestyle Modifications
Making healthy lifestyle choices is crucial for managing heart failure. Recommendations include:
- Dietary adjustments: Consuming a heart-healthy diet low in sodium, saturated fats, and processed foods can help reduce fluid retention and lower blood pressure.
- Regular physical activity: Engaging in moderate exercise, as advised by a healthcare provider, can strengthen the heart and improve overall fitness.
- Weight management: Maintaining a healthy weight reduces strain on the heart and lowers the risk of related conditions.
- Smoking cessation: Quitting smoking improves cardiovascular health and reduces the risk of further heart damage.
- Limiting alcohol intake: Excessive alcohol consumption can worsen heart failure symptoms and should be avoided.
Medications
Several medications are commonly prescribed to manage heart failure and its symptoms:
- Angiotensin-converting enzyme inhibitors: These drugs help relax blood vessels, reducing the workload on the heart.
- Beta-blockers: By slowing the heart rate and reducing blood pressure, beta-blockers allow the heart to pump more efficiently.
- Diuretics: Often referred to as “water pills,” diuretics help eliminate excess fluid from the body, relieving swelling and shortness of breath.
- Aldosterone antagonists: These medications reduce fluid retention and protect the heart from further damage.
- Digoxin: This drug strengthens the heart’s contractions and helps control irregular heart rhythms.
Surgical and Device-Based Treatments
In advanced cases of heart failure, surgical interventions or implantable devices may be necessary:
- Coronary artery bypass surgery: This procedure restores blood flow to the heart by bypassing blocked arteries.
- Heart valve repair or replacement: Correcting faulty heart valves can improve heart function and alleviate symptoms.
- Implantable cardioverter-defibrillators: These devices monitor heart rhythm and deliver shocks if dangerous arrhythmias occur.
- Left ventricular assist devices: Mechanical pumps that help the heart pump blood are used in severe cases or as a bridge to heart transplantation.
- Heart transplantation: For eligible patients with end-stage heart failure, a heart transplant may be considered.
Preventing Heart Failure
While not all cases of heart failure can be prevented, adopting a heart-healthy lifestyle can significantly reduce the risk. Strategies include:
- Controlling high blood pressure: Regular monitoring and treatment can prevent long-term damage to the heart.
- Managing diabetes: Keeping blood sugar levels under control protects against complications that affect the heart.
- Staying physically active: Regular exercise promotes cardiovascular health and reduces the risk of obesity.
- Avoiding tobacco use: Smoking cessation is one of the most effective ways to protect heart health.
- Getting regular check-ups: Routine medical evaluations can detect early signs of heart disease and allow for timely intervention.
By understanding the complexities of heart failure and taking proactive measures, individuals can better manage their condition and improve their overall well-being.