Gestational diabetes mellitus, commonly abbreviated as GDM, is a condition that affects pregnant women, leading to high blood sugar levels. This type of diabetes typically develops during the second or third trimester of pregnancy and usually resolves after childbirth. However, it can pose risks to both the mother and the baby if not managed properly. In this article, we will explore the causes, symptoms, and management strategies for gestational diabetes during pregnancy.
What is Gestational Diabetes?
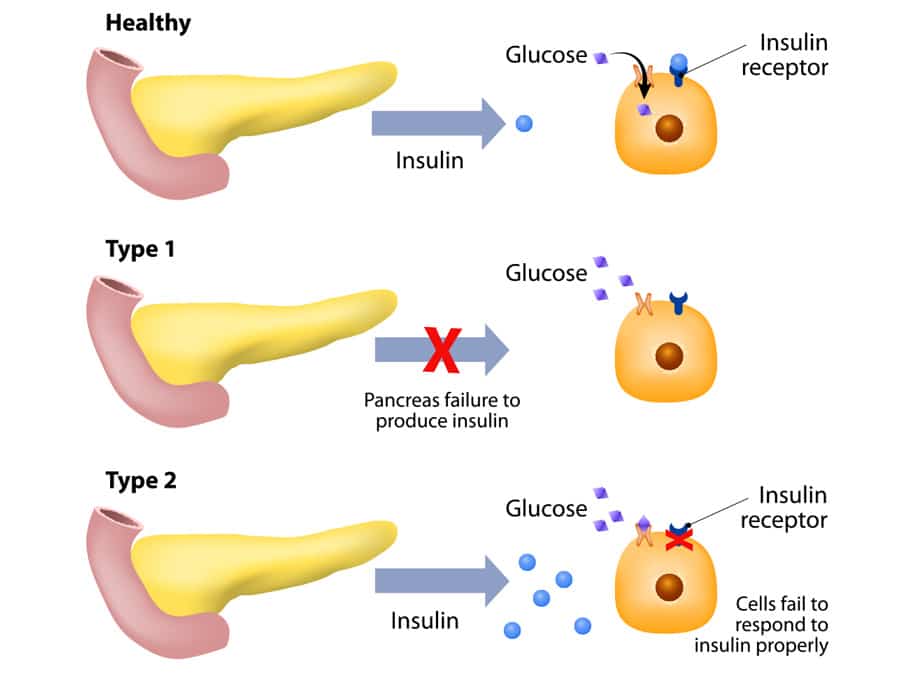
Gestational diabetes is a form of diabetes that occurs exclusively during pregnancy. Unlike other types of diabetes, it does not usually present itself before pregnancy and often disappears after the baby is born. It occurs when the body is unable to produce enough insulin to meet the increased demands during pregnancy. Insulin is a hormone that helps regulate blood sugar levels, and when the body cannot produce sufficient amounts, blood sugar levels rise, leading to gestational diabetes.
Why Does Gestational Diabetes Occur?
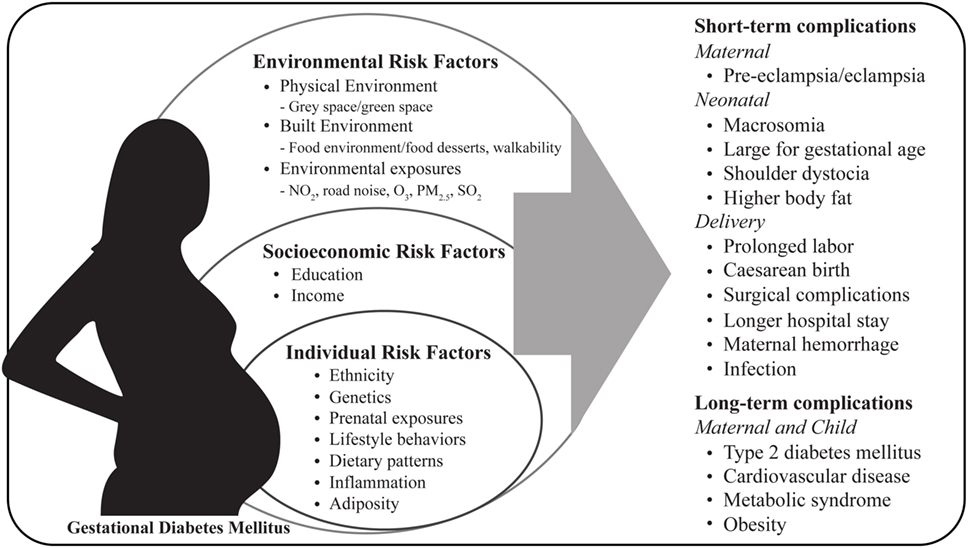
The exact cause of gestational diabetes is not fully understood, but several factors contribute to its development:
- Hormonal Changes: During pregnancy, the placenta produces hormones that help the baby grow and develop. However, these hormones can also interfere with the action of insulin in the mother’s body, leading to insulin resistance.
- Weight Gain: Excessive weight gain during pregnancy can increase the risk of developing gestational diabetes. Extra weight can make it harder for the body to use insulin effectively.
- Genetic Predisposition: Women with a family history of diabetes are more likely to develop gestational diabetes. If a close relative, such as a parent or sibling, has diabetes, the risk increases.
- Previous Pregnancies: Women who have had gestational diabetes in a previous pregnancy are at a higher risk of developing it again in subsequent pregnancies.
- Age: Women over the age of 25 are more likely to develop gestational diabetes, particularly if they are older than 35.
Symptoms of Gestational Diabetes
Gestational diabetes often does not present noticeable symptoms, which is why screening during pregnancy is crucial. However, some women may experience the following signs:
- Increased Thirst: Women with gestational diabetes may feel unusually thirsty, even after drinking plenty of fluids.
- Frequent Urination: High blood sugar levels can lead to increased urination as the body tries to eliminate excess glucose through urine.
- Fatigue: Feeling tired or exhausted despite getting adequate rest can be a sign of uncontrolled blood sugar levels.
- Blurred Vision: Elevated blood sugar levels can cause temporary changes in vision, leading to blurred eyesight.
- Recurrent Infections: High blood sugar levels can weaken the immune system, making women more susceptible to infections such as urinary tract infections or yeast infections.
It is important to note that many of these symptoms are common during pregnancy and may not necessarily indicate gestational diabetes. Therefore, routine screening is essential to detect the condition early.
Risks Associated with Gestational Diabetes
If left untreated, gestational diabetes can lead to complications for both the mother and the baby. Some of the potential risks include:
Risks to the Baby
- Macrosomia: Babies born to mothers with gestational diabetes may be larger than average, a condition known as macrosomia. This can increase the risk of complications during delivery, such as shoulder dystocia or the need for a cesarean section.
- Hypoglycemia: After birth, babies may experience low blood sugar levels because their bodies continue to produce extra insulin in response to the mother’s high blood sugar levels during pregnancy.
- Respiratory Distress Syndrome: Babies born to mothers with poorly controlled gestational diabetes may have difficulty breathing due to underdeveloped lungs.
- Increased Risk of Type 2 Diabetes: Children born to mothers with gestational diabetes are at a higher risk of developing type 2 diabetes later in life.
Risks to the Mother
- Preeclampsia: Women with gestational diabetes are at an increased risk of developing preeclampsia, a condition characterized by high blood pressure and damage to organs such as the liver and kidneys.
- Type 2 Diabetes: Women who develop gestational diabetes are more likely to develop type 2 diabetes later in life, especially if they do not maintain a healthy lifestyle after pregnancy.
- Difficult Delivery: The risk of complications during labor and delivery increases if the baby is larger than average or if the mother requires a cesarean section.
Diagnosis of Gestational Diabetes
Gestational diabetes is typically diagnosed through routine screening during pregnancy. Most healthcare providers recommend testing between 24 and 28 weeks of pregnancy, although women at higher risk may be tested earlier. The most common diagnostic tests include:
Glucose Challenge Test
This initial test involves drinking a sugary solution and having blood drawn an hour later to measure blood sugar levels. If the results are higher than normal, a follow-up test is required.
Oral Glucose Tolerance Test
This more comprehensive test involves fasting overnight, drinking a sugary solution, and having blood drawn multiple times over a few hours to monitor how the body processes glucose. A diagnosis of gestational diabetes is made if blood sugar levels exceed certain thresholds.
Management of Gestational Diabetes
Managing gestational diabetes is crucial to ensure a healthy pregnancy and reduce the risk of complications. The primary goal is to keep blood sugar levels within a target range. This can often be achieved through lifestyle modifications, though some women may require medication.
Dietary Adjustments
A healthy diet plays a key role in managing gestational diabetes. Women are encouraged to work with a registered dietitian to create a meal plan that meets their nutritional needs while keeping blood sugar levels stable. Key dietary recommendations include:
- Carbohydrate Control: Carbohydrates have the most significant impact on blood sugar levels. Women should focus on consuming complex carbohydrates, such as whole grains, vegetables, and legumes, while limiting refined carbohydrates like white bread and sugary snacks.
- Protein Intake: Including lean protein sources, such as poultry, fish, tofu, and legumes, can help stabilize blood sugar levels and promote satiety.
- Healthy Fats: Incorporating healthy fats, such as those found in avocados, nuts, seeds, and olive oil, can support overall health without spiking blood sugar levels.
- Regular Meals: Eating small, frequent meals throughout the day can help prevent blood sugar spikes and crashes.
Physical Activity
Regular physical activity is another important component of managing gestational diabetes. Exercise helps the body use insulin more effectively and can lower blood sugar levels. Safe activities for pregnant women include:
- Walking: A simple and effective way to stay active during pregnancy.
- Swimming: A low-impact exercise that is gentle on the joints.
- Prenatal Yoga: Helps improve flexibility, strength, and relaxation.
- Strength Training: Light resistance exercises using weights or resistance bands can help build muscle and improve insulin sensitivity.
Women should consult their healthcare provider before starting any exercise program to ensure it is safe for their specific situation.
Blood Sugar Monitoring
Regular monitoring of blood sugar levels is essential for managing gestational diabetes. Women may be asked to check their blood sugar levels multiple times a day, including fasting levels in the morning and after meals. Keeping a log of these readings can help healthcare providers adjust treatment plans as needed.
Medication
In some cases, lifestyle changes alone may not be sufficient to control blood sugar levels. Women with gestational diabetes may require medication to help manage their condition. Options include:
- Insulin Therapy: Insulin injections are the most common form of medication for gestational diabetes. They are safe for both the mother and the baby and can be adjusted based on blood sugar levels.
- Oral Medications: In certain cases, oral medications may be prescribed to help lower blood sugar levels. However, insulin is generally preferred for gestational diabetes.
Postpartum Care and Long-Term Health
After giving birth, most women with gestational diabetes see their blood sugar levels return to normal. However, it is important to continue monitoring blood sugar levels in the weeks following delivery to ensure they remain within a healthy range. Additionally, women who have had gestational diabetes are at an increased risk of developing type 2 diabetes later in life. To reduce this risk, they should:
- Maintain a healthy weight through a balanced diet and regular exercise.
- Undergo regular screenings for diabetes, as recommended by their healthcare provider.
- Adopt a proactive approach to overall health and wellness.
By taking these steps, women can significantly reduce their risk of developing type 2 diabetes and promote long-term health for themselves and their families.