Genital herpes, caused by the herpes simplex virus type two, is a prevalent sexually transmitted infection that affects millions of people worldwide. This condition not only impacts physical health but also has profound emotional and psychological effects on those who live with it. Understanding its causes, symptoms, transmission, diagnosis, treatment, and prevention is essential for managing the condition effectively and reducing its spread.
What Is Genital Herpes?
Genital herpes is a viral infection that primarily affects the genital and anal areas. It is caused by a specific type of virus known as herpes simplex virus type two. This virus belongs to the same family as the virus responsible for cold sores, which is called herpes simplex virus type one. While both types can cause infections in either location, herpes simplex virus type two is most commonly associated with genital infections.
The infection is characterized by outbreaks of painful blisters or sores in the affected areas. These outbreaks can occur intermittently, often triggered by factors such as stress, illness, or hormonal changes. Despite being incurable, the condition can be managed with proper care and medical intervention.
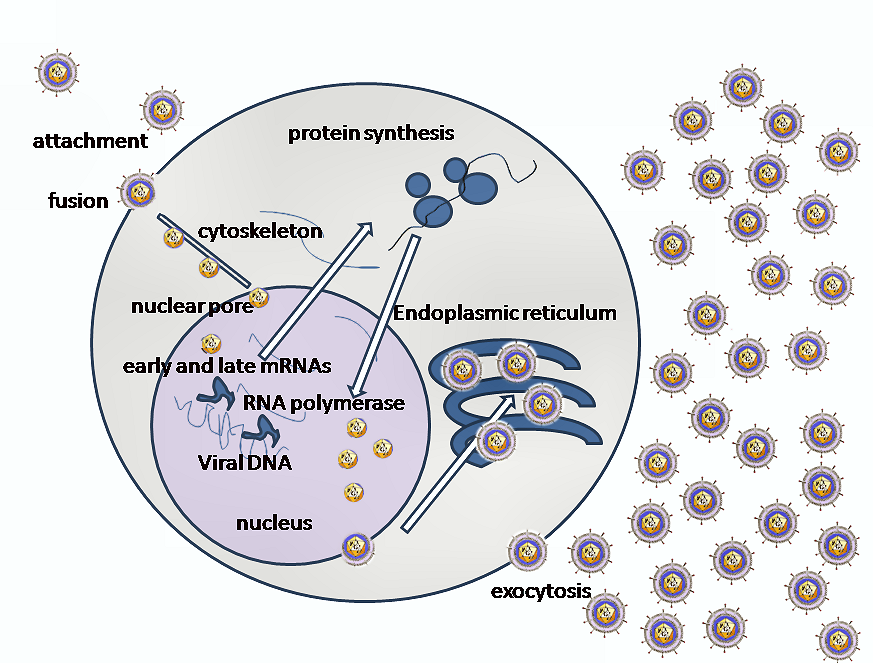
How Does the Infection Develop?
The virus enters the body through small breaks in the skin or mucous membranes during sexual contact. Once inside, it travels to nerve cells near the spine, where it remains dormant until triggered. During an outbreak, the virus reactivates, travels back to the skin, and causes visible symptoms.
Symptoms of Genital Herpes
The symptoms of this condition can vary widely from person to person. Some individuals may experience severe symptoms, while others may have mild or no noticeable signs at all. Recognizing these symptoms is crucial for seeking timely medical attention and preventing further transmission.
Initial Symptoms
- Pain or itching: Before the appearance of sores, individuals may feel discomfort, tingling, or burning sensations in the genital or anal area.
- Blisters: Small, fluid-filled blisters may develop on or around the genitals, anus, thighs, or buttocks. These blisters can burst, leaving painful ulcers.
- Ulcers: After the blisters rupture, open sores or ulcers form, which can take several weeks to heal.
Other Possible Symptoms
- Flu-like symptoms: Some individuals may experience fever, headache, muscle aches, or swollen lymph nodes during their first outbreak.
- Painful urination: The presence of sores can make urination uncomfortable or painful.
- Vaginal or penile discharge: Unusual discharge may occur in some cases.
Recurrent Outbreaks
After the initial infection, the virus remains in the body and can cause recurrent outbreaks. These episodes are usually less severe than the first outbreak and may become less frequent over time. Triggers for recurrent outbreaks include stress, fatigue, illness, hormonal fluctuations, or exposure to ultraviolet light.
Transmission of Genital Herpes
This condition is highly contagious and spreads through direct skin-to-skin contact during sexual activity. Understanding how the infection is transmitted is vital for preventing its spread to others.
Sexual Contact
The virus can be transmitted through vaginal, anal, or oral sex. Even when no visible symptoms are present, the virus can still be shed from the skin and infect a partner. This is known as asymptomatic viral shedding.
Non-Sexual Transmission
In rare cases, the infection can be transmitted through non-sexual means, such as sharing towels or clothing contaminated with the virus. However, this mode of transmission is uncommon.
Risk Factors
- Unprotected sex: Engaging in sexual activity without using protection increases the risk of transmission.
- Multiple partners: Having multiple sexual partners raises the likelihood of exposure to the virus.
- Weakened immune system: Individuals with compromised immune systems are more susceptible to infection.
Diagnosis of Genital Herpes
Accurate diagnosis is essential for effective management of the condition. If you suspect you have been exposed to the virus or are experiencing symptoms, it is important to consult a healthcare provider for evaluation.
Clinical Examination
A healthcare provider will typically perform a physical examination to assess the presence of sores or other symptoms. They may also inquire about your medical history and sexual activity to better understand your risk factors.
Laboratory Tests
To confirm the diagnosis, laboratory tests are often required. These tests may include:
- Viral culture: A sample is taken from a sore and tested for the presence of the virus.
- Polymerase chain reaction (PCR) test: This test detects the genetic material of the virus in a sample and is highly accurate.
- Blood test: A blood sample can be analyzed for antibodies to determine if you have been infected with the virus.
Treatment Options for Genital Herpes
While there is no cure for this condition, various treatments are available to manage symptoms, reduce the frequency of outbreaks, and lower the risk of transmission to others.
Antiviral Medications
Antiviral medications are the primary treatment for managing this condition. These drugs work by suppressing the activity of the virus and reducing the severity and duration of outbreaks. Commonly prescribed antiviral medications include:
- Acyclovir: One of the oldest and most widely used antiviral drugs for treating this condition.
- Valacyclovir: A prodrug of acyclovir that is more convenient to take due to less frequent dosing.
- Famciclovir: Another antiviral medication that helps control outbreaks and reduce symptoms.
Dosage and Administration
These medications can be taken in different ways depending on the individual’s needs:
- Episodic therapy: Medications are taken only during outbreaks to shorten their duration and alleviate symptoms.
- Suppressive therapy: Daily medication is taken to reduce the frequency of outbreaks and lower the risk of transmission to partners.
Pain Relief Measures
In addition to antiviral medications, over-the-counter pain relievers such as acetaminophen or ibuprofen can help manage discomfort during outbreaks. Topical treatments, such as creams or ointments, may also provide relief for localized pain.
Prevention Strategies
Preventing the spread of this condition requires a combination of safe sexual practices, regular testing, and open communication with sexual partners.
Safe Sexual Practices
- Use condoms: Consistently using latex or polyurethane condoms during sexual activity can significantly reduce the risk of transmission.
- Avoid sex during outbreaks: Refrain from sexual activity when symptoms are present to prevent spreading the virus.
- Consider suppressive therapy: Taking daily antiviral medications can reduce the risk of transmitting the virus to partners.
Regular Testing
Regular screening for sexually transmitted infections, including this condition, is important, especially for individuals with multiple partners or those in new relationships. Early detection allows for timely treatment and reduces the risk of spreading the infection.
Education and Awareness
Raising awareness about this condition and promoting education about safe sexual practices can help reduce stigma and encourage individuals to seek testing and treatment. Open discussions with healthcare providers and partners are essential for fostering understanding and support.
Living with Genital Herpes
Living with this condition involves more than just managing physical symptoms. Emotional and psychological well-being are equally important aspects of coping with the infection.
Emotional Impact
Many individuals experience feelings of shame, guilt, or anxiety after being diagnosed with this condition. Seeking support from mental health professionals, support groups, or trusted friends and family members can help address these emotions and improve overall quality of life.
Healthy Lifestyle Choices
Maintaining a healthy lifestyle can help strengthen the immune system and reduce the frequency of outbreaks. This includes eating a balanced diet, exercising regularly, managing stress, and getting adequate sleep.
Building Strong Relationships
Open and honest communication with sexual partners is crucial for maintaining trust and preventing misunderstandings. Discussing the condition openly and providing accurate information can help partners make informed decisions about their sexual health.
Research and Future Directions
Ongoing research into this condition aims to improve diagnostic tools, develop more effective treatments, and explore potential vaccines. Advances in medical science hold promise for better management and, ultimately, a cure for this persistent infection.
New Treatment Approaches
Scientists are investigating novel antiviral therapies and immunotherapies that target the virus more effectively. These innovations could lead to longer-lasting suppression of the virus and fewer side effects for patients.
Vaccine Development
Efforts to create a vaccine for this condition are ongoing. A successful vaccine could prevent new infections and reduce the global burden of the disease.
Improved Diagnostic Tools
Enhanced diagnostic methods, such as faster and more accurate tests, could facilitate earlier detection and treatment, improving outcomes for individuals with the condition.