Foot drop, also known as drop foot, is a medical condition characterized by the inability to lift the front part of the foot. This leads to difficulty in walking and often results in dragging the toes along the ground. Foot drop is not a disease itself but rather a symptom of an underlying problem involving nerves, muscles, or the brain. It can affect one or both feet and may arise from a variety of causes, including neurological disorders, injuries, or structural abnormalities. Understanding the causes, symptoms, diagnosis, and treatment options for this condition is essential for managing it effectively.
What Causes Foot Drop?
The primary cause of foot drop is weakness or paralysis of the muscles responsible for lifting the foot. These muscles are controlled by the peroneal nerve, which runs along the leg and is susceptible to damage. Below are some common causes of foot drop:
1. Nerve Injuries
- Trauma: Accidents such as fractures, dislocations, or surgeries around the knee or lower leg can damage the peroneal nerve.
- Compression: Prolonged pressure on the nerve, such as from crossing legs or wearing tight casts, can lead to nerve dysfunction.
2. Neurological Disorders
- Multiple Sclerosis: A chronic condition that affects the central nervous system, leading to muscle weakness and coordination issues.
- Stroke: A sudden interruption of blood flow to the brain can impair motor control and result in foot drop.
- Amyotrophic Lateral Sclerosis: Also known as Lou Gehrig’s disease, this condition causes progressive muscle weakness and loss of function.
3. Muscle Disorders
- Muscular Dystrophy: A group of genetic diseases that weaken and break down muscles over time.
- Poliomyelitis: A viral infection that damages motor neurons, causing muscle paralysis.
4. Spinal Conditions
- Herniated Discs: Bulging discs in the spine can compress nerves that control foot movement.
- Spinal Stenosis: Narrowing of the spinal canal can put pressure on nerves, leading to foot drop.
Symptoms of Foot Drop
Foot drop manifests through specific signs and symptoms that can vary in severity depending on the underlying cause. Some common symptoms include:
- Dragging of the Foot: The most noticeable symptom is the inability to lift the front part of the foot, causing it to drag along the ground while walking.
- High Steppage Gait: To compensate for the inability to lift the foot, individuals may raise their knees higher than normal while walking, resembling a marching gait.
- Tripping: The toes may catch on uneven surfaces or carpets, increasing the risk of falls.
- Numbness or Tingling: Sensory changes in the affected foot or leg may occur due to nerve involvement.
- Weakness: Reduced strength in the muscles responsible for lifting the foot is a hallmark of this condition.
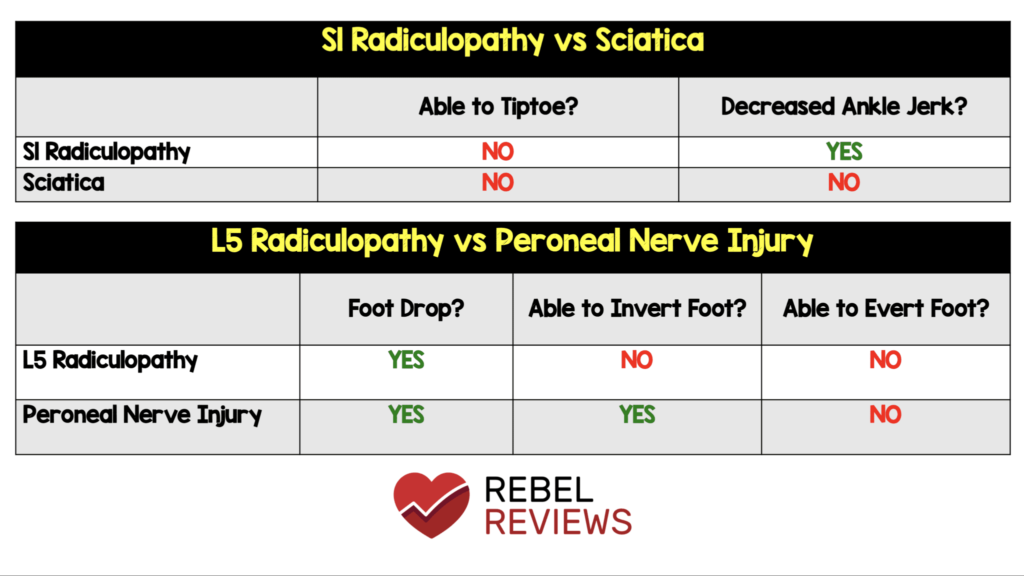
Diagnosing Foot Drop
Diagnosing foot drop involves a comprehensive evaluation to identify its root cause. Healthcare providers typically use a combination of physical examinations, imaging studies, and specialized tests to determine the underlying issue. Here’s how the diagnostic process generally unfolds:
1. Physical Examination
During a physical examination, the healthcare provider assesses muscle strength, reflexes, and sensation in the affected leg and foot. They may also observe the patient’s gait to identify any abnormalities, such as dragging or high steppage gait.
2. Medical History
Understanding the patient’s medical history is crucial. Questions about recent injuries, surgeries, or existing conditions like diabetes or multiple sclerosis can provide valuable clues about the cause of foot drop.
3. Imaging Studies
- X-rays: These can help detect fractures, dislocations, or other structural abnormalities in the leg or spine.
- Magnetic Resonance Imaging: MRI scans provide detailed images of soft tissues, including nerves and muscles, to identify compression or damage.
- Ultrasound: This non-invasive test can visualize the peroneal nerve and detect any irregularities.
4. Electromyography and Nerve Conduction Studies
These tests measure the electrical activity of muscles and the speed at which nerves transmit signals. They are particularly useful in diagnosing nerve damage or dysfunction.
Treatment Options for Foot Drop
Treatment for foot drop depends on its underlying cause and severity. While some cases may resolve with time, others require long-term management. Below are the main treatment approaches:
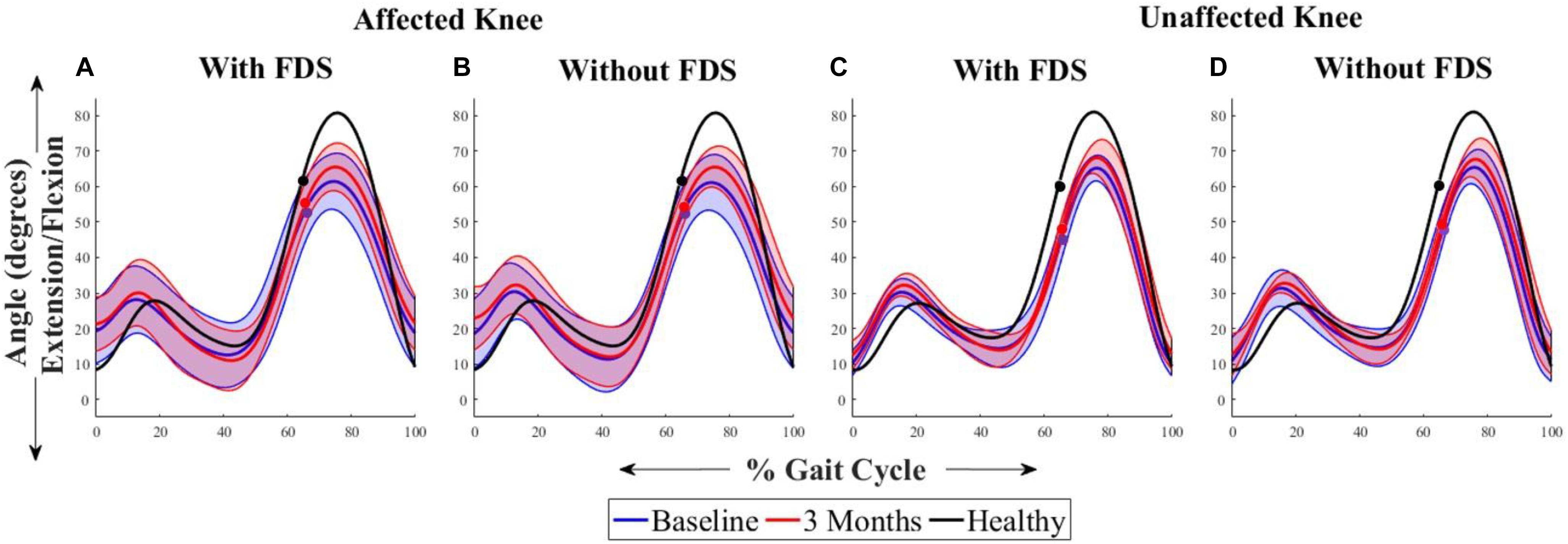
1. Physical Therapy
Physical therapy plays a vital role in improving muscle strength, flexibility, and coordination. Therapists may recommend exercises to strengthen the muscles involved in lifting the foot and stretches to prevent stiffness. Gait training can also help patients learn to walk more safely and efficiently.
2. Assistive Devices
- Ankle-Foot Orthosis: This brace supports the foot and ankle, keeping the foot in a neutral position and preventing it from dragging.
- Canes or Walkers: These devices provide stability and reduce the risk of falls for individuals with severe foot drop.
3. Medications
In cases where foot drop is caused by inflammation or nerve compression, medications such as anti-inflammatory drugs or corticosteroids may be prescribed to reduce swelling and alleviate symptoms.
4. Surgery
Surgical intervention may be necessary if foot drop results from structural abnormalities or severe nerve damage. Procedures can include:
- Nerve Decompression: Relieving pressure on the affected nerve to restore function.
- Nerve Repair or Grafting: Reconnecting or replacing damaged nerves to improve signal transmission.
- Tendon Transfer: Repositioning tendons to enhance foot movement when nerve repair is not feasible.
5. Electrical Stimulation
Functional electrical stimulation involves using a device to deliver electrical impulses to the muscles responsible for lifting the foot. This can help retrain the muscles and improve mobility.
6. Addressing Underlying Conditions
If foot drop is a symptom of a broader medical condition, treating the primary issue is essential. For example, managing diabetes, undergoing physical rehabilitation after a stroke, or receiving treatment for multiple sclerosis can help alleviate foot drop symptoms.
Lifestyle Modifications and Preventive Measures
In addition to medical treatments, certain lifestyle changes can help manage foot drop and prevent further complications:
- Regular Exercise: Engaging in low-impact activities like swimming or cycling can improve overall muscle strength and flexibility.
- Proper Footwear: Wearing supportive shoes with adequate cushioning can reduce discomfort and improve stability.
- Avoiding Prolonged Pressure: Taking breaks from sitting positions that compress the peroneal nerve can prevent nerve damage.
- Home Safety Measures: Removing tripping hazards and installing handrails can create a safer environment for individuals with foot drop.