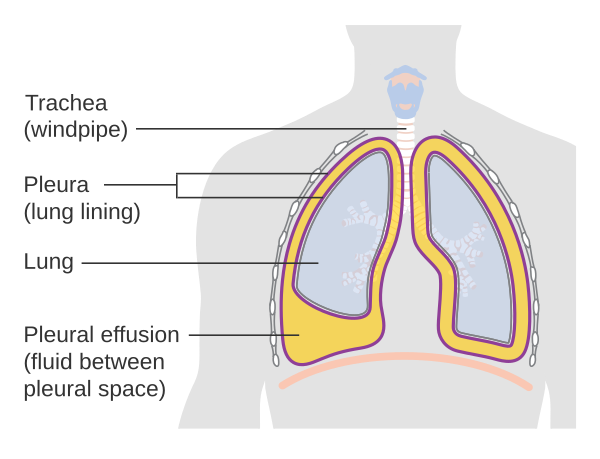
Pleural effusion, commonly abbreviated as PE, refers to the accumulation of excess fluid in the pleural space, which is the thin layer between the lungs and the chest wall. This condition can significantly impact breathing and may signal an underlying health issue. Understanding its causes, diagnosis, and treatment options is essential for effective management. In this article, we will explore all aspects of fluid around the lungs in detail.
What is Fluid Around the Lungs?
The pleural space is a small cavity that contains a minimal amount of lubricating fluid. This fluid allows the lungs to glide smoothly against the chest wall during breathing. However, when there is an abnormal buildup of fluid in this space, it leads to pleural effusion. The excess fluid can compress the lungs, making it difficult to breathe and causing discomfort or pain.
Types of Pleural Effusion
- Transudative Effusion: This type occurs when there is an imbalance in the pressure within blood vessels or low protein levels in the blood. It is often associated with conditions like heart failure or liver disease.
- Exudative Effusion: This type results from inflammation or damage to the pleura, leading to leakage of fluid, protein, or even blood into the pleural space. Common causes include infections, cancer, or lung injuries.
Causes of Fluid Accumulation Around the Lungs
Pleural effusion can arise from a wide range of medical conditions. Some of the most common causes are outlined below:
Cardiac Conditions
Heart failure is one of the leading causes of transudative pleural effusion. When the heart cannot pump blood effectively, fluid can back up into the veins, increasing pressure in the blood vessels around the lungs. This pressure forces fluid to leak into the pleural space.
Infections
Infections such as pneumonia or tuberculosis can cause inflammation of the pleura, leading to exudative effusion. Bacterial, viral, or fungal infections can irritate the lining of the lungs, prompting the body to produce excess fluid as part of the immune response.
Cancer
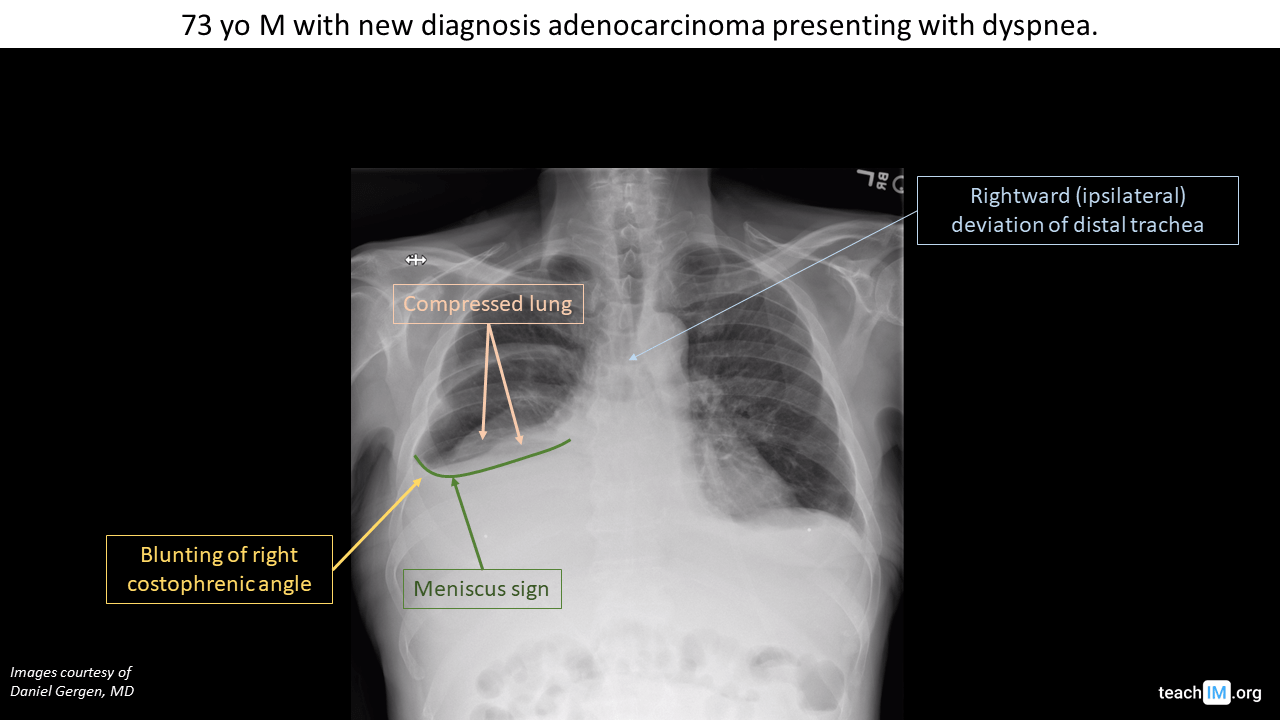
Certain types of cancer, including lung cancer and breast cancer, can spread to the pleura and cause fluid buildup. Additionally, cancers of the blood, such as lymphoma or leukemia, may also lead to pleural effusion.
Liver and Kidney Diseases
Liver cirrhosis and kidney failure can result in low protein levels in the blood, leading to transudative effusion. These conditions affect the body’s ability to maintain fluid balance, causing fluid to accumulate in various parts of the body, including the pleural space.
Pulmonary Embolism
A pulmonary embolism occurs when a blood clot blocks a vessel in the lungs. This condition can trigger inflammation and fluid accumulation in the pleural space, contributing to pleural effusion.
Autoimmune Disorders
Diseases like rheumatoid arthritis and lupus can cause inflammation of the pleura, resulting in exudative effusion. These autoimmune conditions cause the immune system to mistakenly attack healthy tissues, including the lining of the lungs.
Symptoms of Fluid Around the Lungs
The symptoms of pleural effusion can vary depending on the severity of the fluid buildup and the underlying cause. Some individuals may not experience noticeable symptoms, while others may have significant discomfort. Common signs include:
- Shortness of breath, especially during physical activity
- Chest pain, often worsened by deep breathing or coughing
- Dry cough
- Rapid breathing
- Fatigue or weakness
- Fever, if the effusion is caused by an infection
Diagnosis of Pleural Effusion
Diagnosing fluid around the lungs involves a combination of physical examination, imaging tests, and laboratory analysis. Here are the key steps involved in the diagnostic process:
Physical Examination
A healthcare provider may listen to the patient’s lungs using a stethoscope. Reduced or absent breath sounds on one side of the chest can indicate the presence of fluid. Additionally, percussion of the chest may reveal dullness over areas where fluid has accumulated.
Imaging Tests
- Chest X-ray: A chest X-ray is often the first test used to detect pleural effusion. It can show the presence of fluid and help estimate its volume.
- Ultrasound: An ultrasound provides a more detailed view of the pleural space and can guide procedures like thoracentesis, which involves removing fluid for analysis.
- CT Scan: A computed tomography scan offers a comprehensive image of the chest, helping identify the underlying cause of the effusion.
Thoracentesis
Thoracentesis is a procedure in which a needle is inserted into the pleural space to remove fluid. The collected fluid is then analyzed in a laboratory to determine whether it is transudative or exudative. This distinction is crucial for identifying the underlying cause of the effusion.
Blood Tests
Blood tests may be performed to check for infections, autoimmune disorders, or abnormalities in organ function. These tests can provide additional clues about the root cause of the fluid buildup.
Treatment Options for Pleural Effusion
The treatment of fluid around the lungs depends on the underlying cause, the severity of symptoms, and the type of effusion. Below are some common approaches to managing pleural effusion:
Treating the Underlying Cause
Addressing the root cause of the effusion is essential for long-term management. For example:
- Heart failure may require medications like diuretics to reduce fluid retention.
- Infections may be treated with antibiotics or antiviral drugs.
- Cancer-related effusions may involve chemotherapy, radiation therapy, or surgery.
Draining the Fluid
In cases where the fluid buildup is significant and causing symptoms, draining the fluid may be necessary. This can be achieved through:
- Thoracentesis: As mentioned earlier, this procedure removes fluid for both diagnostic and therapeutic purposes.
- Chest Tube Insertion: A chest tube may be placed to continuously drain large amounts of fluid over several days.
- Pleurodesis: This procedure involves injecting a substance into the pleural space to prevent fluid from reaccumulating. It is often used for recurrent effusions.
Oxygen Therapy
If the patient is experiencing difficulty breathing due to the effusion, supplemental oxygen may be provided to improve oxygen levels in the blood.
Pain Management
Chest pain associated with pleural effusion can be managed with over-the-counter pain relievers or prescription medications, depending on the severity of the discomfort.
Preventing Recurrence of Pleural Effusion
Preventing the recurrence of fluid around the lungs involves addressing the underlying condition and adopting lifestyle changes to support overall health. Some preventive measures include:
- Managing chronic conditions like heart failure, liver disease, or kidney disease through medication and regular monitoring.
- Avoiding smoking and exposure to environmental toxins to reduce the risk of lung infections and cancer.
- Maintaining a healthy diet and staying physically active to support immune function and overall well-being.
When to Seek Medical Attention
If you experience any of the following symptoms, it is important to seek medical attention promptly:
- Sudden or worsening shortness of breath
- Severe chest pain
- High fever or chills
- Coughing up blood
These symptoms may indicate a serious underlying condition that requires immediate evaluation and treatment.