Fetal macrosomia, often abbreviated as FM, is a condition in which a newborn weighs significantly more than average at birth. Typically, this means the baby weighs over 4,000 grams (approximately 8 pounds, 13 ounces) or more. This condition can pose challenges during pregnancy, labor, and delivery for both the mother and the baby. Understanding its causes, how it is diagnosed, and the available delivery options can help parents and healthcare providers make informed decisions to ensure the best possible outcomes.
What Is Fetal Macrosomia?
Fetal macrosomia refers to an infant who is larger than expected for their gestational age. While there is no universally agreed-upon weight threshold, most healthcare professionals consider a newborn weighing over 4,000 grams to have fetal macrosomia. In some cases, babies may weigh even more, exceeding 4,500 grams (about 9 pounds, 15 ounces). These larger-than-average infants are at higher risk for complications during childbirth and may require special care after delivery.
Causes of Fetal Macrosomia
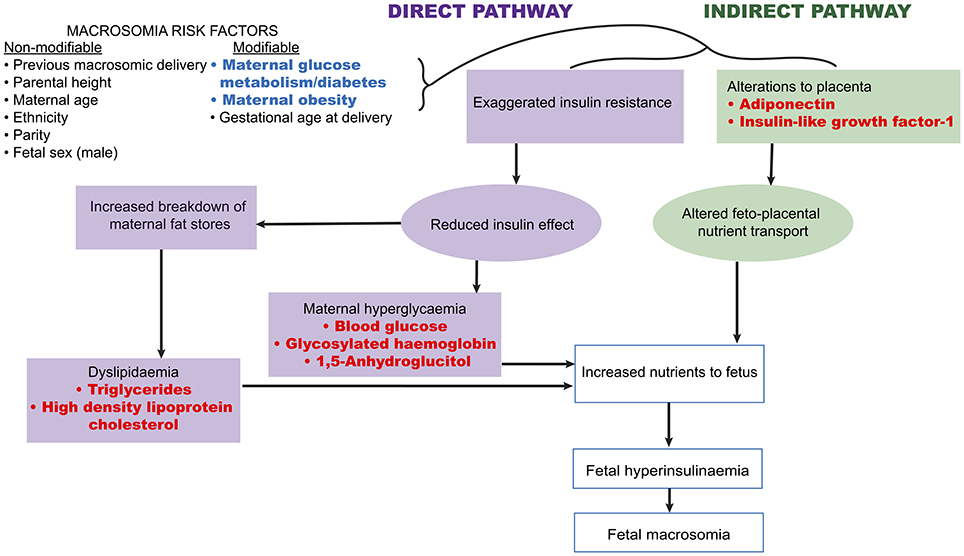
The exact cause of fetal macrosomia is not always clear, but several factors are known to contribute to the condition. These include maternal health, genetic factors, and lifestyle choices. Below are some of the primary causes:
Maternal Diabetes
- Gestational Diabetes: When a pregnant woman develops diabetes during pregnancy, it can lead to excessive growth of the fetus. High blood sugar levels in the mother can cross the placenta, causing the baby’s pancreas to produce extra insulin. This excess insulin can result in increased fat storage and overall growth.
- Pregestational Diabetes: Women who have diabetes before becoming pregnant are also at a higher risk of having a baby with fetal macrosomia. Proper management of blood sugar levels before and during pregnancy is crucial to minimizing this risk.
Genetic Factors
- Family History: If either parent was born large or has a history of giving birth to large babies, there may be a genetic predisposition to fetal macrosomia.
- Racial and Ethnic Background: Certain ethnic groups, such as Hispanic women, tend to have a higher incidence of fetal macrosomia compared to others.
Maternal Weight and Lifestyle
- Obesity: Women who are overweight or obese before pregnancy are more likely to have larger babies. Excess maternal weight can lead to increased nutrient availability for the fetus, promoting excessive growth.
- Excessive Weight Gain During Pregnancy: Gaining more weight than recommended during pregnancy can also contribute to fetal macrosomia.
Post-Term Pregnancy
Pregnancies that extend beyond the expected due date can increase the likelihood of fetal macrosomia. The longer the pregnancy continues, the more time the fetus has to grow, potentially leading to excessive size.
Diagnosing Fetal Macrosomia
Diagnosing fetal macrosomia can be challenging because it is difficult to accurately predict a baby’s weight before birth. However, healthcare providers use a combination of methods to assess the likelihood of the condition:
Ultrasound Measurements
Ultrasound imaging is one of the most common tools used to estimate fetal size. By measuring various parts of the baby, such as the head, abdomen, and femur, doctors can estimate the baby’s weight. While ultrasounds provide valuable information, they are not always precise, especially in late pregnancy when the margin of error increases.
Fundal Height Measurement
During prenatal visits, healthcare providers often measure the distance from the top of the uterus to the pubic bone, known as the fundal height. If the measurement is larger than expected for the gestational age, it may indicate a larger-than-average baby.
Amniotic Fluid Levels
Higher levels of amniotic fluid, a condition called polyhydramnios, can sometimes be associated with fetal macrosomia. This is because larger babies tend to produce more urine, which contributes to increased fluid levels.
Clinical Judgment
In some cases, healthcare providers rely on their clinical experience and judgment to assess the likelihood of fetal macrosomia. Factors such as the mother’s health, previous pregnancies, and family history can all play a role in forming an accurate diagnosis.
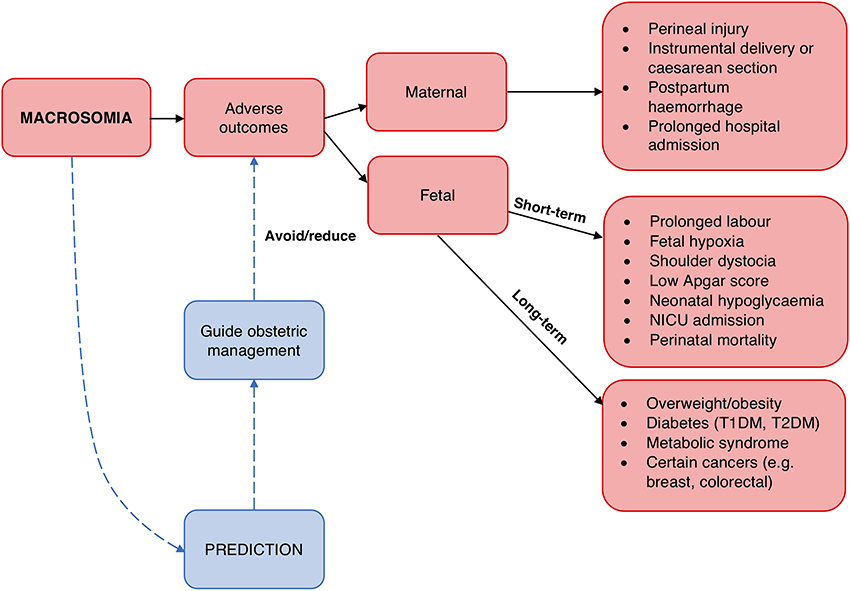
Potential Complications of Fetal Macrosomia
Fetal macrosomia can lead to complications for both the mother and the baby. Understanding these risks is essential for making informed decisions about delivery options.
Complications for the Mother
- Labor Difficulties: Larger babies can make labor more challenging. Prolonged labor and stalled progress are common issues.
- Cesarean Delivery: The risk of needing a cesarean section increases with fetal macrosomia, especially if the baby’s size makes vaginal delivery unsafe.
- Tissue Damage: Vaginal tears and damage to the pelvic floor muscles are more likely with larger babies.
Complications for the Baby
- Shoulder Dystocia: This occurs when the baby’s shoulders get stuck behind the mother’s pelvic bone during delivery. It can lead to nerve damage or fractures in the baby.
- Birth Injuries: Larger babies are at higher risk for injuries such as brachial plexus injuries, which affect the nerves controlling arm movement.
- Hypoglycemia: Babies born to mothers with diabetes are at risk of low blood sugar levels after birth, requiring close monitoring and treatment.
Delivery Options for Fetal Macrosomia
When fetal macrosomia is suspected, healthcare providers will carefully evaluate the best delivery option based on the specific circumstances of the pregnancy. Below are the main delivery options:
Vaginal Delivery
A vaginal delivery may still be possible for some women with fetal macrosomia, depending on factors such as the estimated fetal weight, maternal health, and the baby’s position. However, there are risks involved, including:
- Increased likelihood of shoulder dystocia
- Prolonged labor
- Vaginal tearing or other tissue damage
To mitigate these risks, healthcare providers may recommend interventions such as inducing labor earlier or using assisted delivery techniques like forceps or vacuum extraction.
Cesarean Section
In cases where the risk of complications during vaginal delivery is high, a cesarean section may be recommended. This is particularly true if:
- The estimated fetal weight exceeds 4,500 grams
- The mother has diabetes
- Previous deliveries resulted in shoulder dystocia or other complications
A cesarean section reduces the risk of shoulder dystocia and other birth injuries but comes with its own set of risks, such as infection, blood loss, and longer recovery times for the mother.
Induction of Labor
In some cases, healthcare providers may recommend inducing labor before the due date to reduce the risk of complications. Inducing labor earlier can prevent the baby from growing too large, but it must be carefully timed to avoid premature birth.
Monitoring During Delivery
Regardless of the delivery method chosen, close monitoring during labor and delivery is essential. Continuous fetal heart rate monitoring and careful assessment of the baby’s position can help healthcare providers respond quickly to any complications that arise.
Managing Fetal Macrosomia After Birth
After delivery, babies with fetal macrosomia may require additional care to address potential complications. For example:
- Babies born to mothers with diabetes may need frequent blood sugar checks and treatment for hypoglycemia.
- Infants with birth injuries, such as brachial plexus injuries, may require physical therapy or other interventions to regain full function.
- Close monitoring of feeding and weight gain is important to ensure the baby is thriving.
Preventing Fetal Macrosomia
While not all cases of fetal macrosomia can be prevented, certain steps can reduce the risk:
- Maintain a healthy weight before and during pregnancy
- Manage blood sugar levels carefully if diagnosed with diabetes
- Follow a balanced diet and exercise regularly under medical guidance
- Attend all prenatal appointments to monitor fetal growth
By taking proactive measures, expectant mothers can minimize the likelihood of fetal macrosomia and its associated complications.