A fast heart rate, also known as tachycardia, refers to a condition where the heart beats faster than normal while at rest. In adults, a resting heart rate of more than 100 beats per minute is generally considered abnormal. Tachycardia can occur in various forms and may affect different parts of the heart. While some cases are harmless, others can lead to serious complications if left untreated. This article provides an in-depth look at what tachycardia is, its types, potential causes, and available treatments.
What Is a Fast Heart Rate?
A fast heart rate occurs when the electrical signals that control the heartbeat become disrupted. Normally, the heart’s rhythm is regulated by a natural pacemaker called the sinoatrial node, which sends electrical impulses to coordinate the contractions of the heart chambers. When these signals malfunction or travel abnormally, the heart may beat too quickly, leading to tachycardia.
While many people experience brief episodes of a fast heart rate due to stress, exercise, or other factors, persistent or recurrent tachycardia may indicate an underlying health issue. The severity of symptoms and the impact on overall health can vary depending on the type of tachycardia and the individual’s condition.
Symptoms of a Fast Heart Rate
- Racing heartbeat or palpitations
- Chest pain or discomfort
- Shortness of breath
- Dizziness or lightheadedness
- Fainting or near-fainting episodes
- Fatigue or weakness
In some cases, individuals with a fast heart rate may not experience any noticeable symptoms, especially if the condition is mild or intermittent. However, it is important to seek medical attention if symptoms persist or worsen over time.
Types of Fast Heart Rate
There are several types of tachycardia, each originating from different areas of the heart and characterized by distinct patterns of electrical activity. Understanding the specific type of tachycardia is crucial for determining the appropriate treatment approach.
Atrial Fibrillation
Atrial fibrillation is one of the most common types of fast heart rate. It occurs when the upper chambers of the heart, known as the atria, beat irregularly and often too quickly. This irregular rhythm can disrupt the flow of blood through the heart, increasing the risk of blood clots and stroke. Atrial fibrillation is often associated with conditions such as high blood pressure, heart disease, and thyroid disorders.
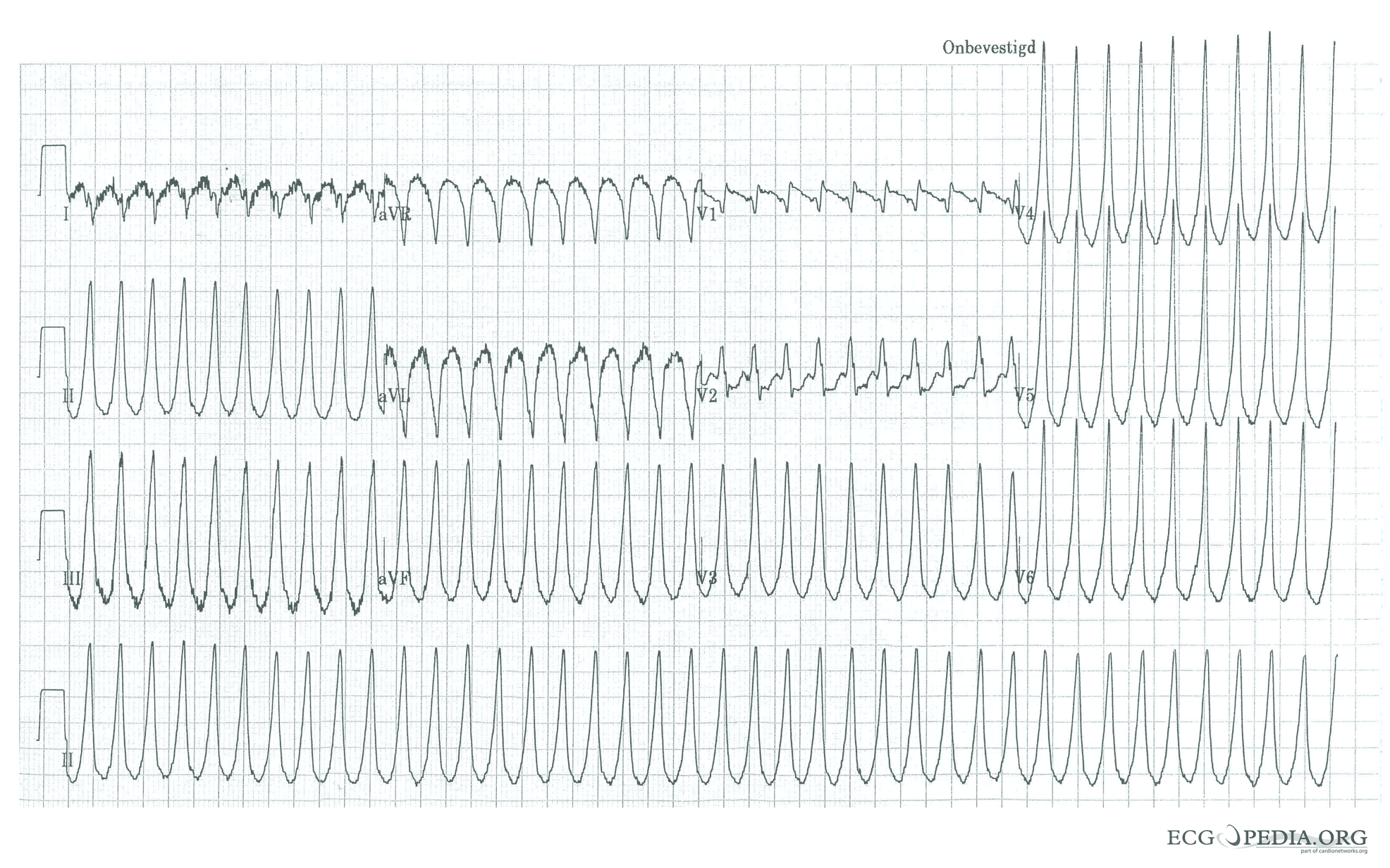
Ventricular Tachycardia
Ventricular tachycardia originates in the lower chambers of the heart, called the ventricles. This type of fast heart rate can be life-threatening because it prevents the heart from pumping blood effectively. Ventricular tachycardia may occur in individuals with structural heart disease, electrolyte imbalances, or a history of heart attacks. Immediate medical intervention is often required to restore a normal rhythm.
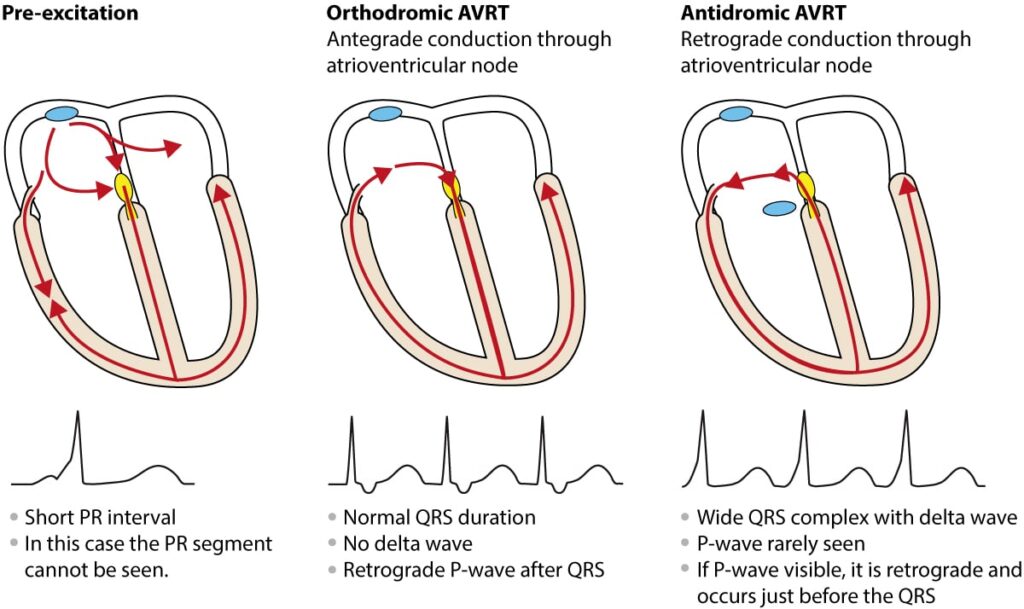
Supraventricular Tachycardia
Supraventricular tachycardia refers to a group of fast heart rhythms that originate above the ventricles, typically in the atria or the atrioventricular node. These episodes often begin and end suddenly and may last from a few seconds to several hours. Supraventricular tachycardia is more common in younger individuals and is often triggered by stress, caffeine, or physical exertion.
Sinus Tachycardia
Sinus tachycardia occurs when the heart’s natural pacemaker increases the heart rate in response to certain stimuli, such as exercise, fever, or emotional stress. Unlike other types of fast heart rate, sinus tachycardia is usually a normal physiological response and does not require treatment unless it persists without an identifiable cause.
Causes of a Fast Heart Rate
The causes of a fast heart rate can vary widely, ranging from lifestyle factors to underlying medical conditions. Identifying the root cause is essential for effective management and treatment.
Lifestyle Factors
Several lifestyle-related factors can contribute to a fast heart rate:
- Excessive consumption of caffeine or alcohol
- Smoking or tobacco use
- Stress or anxiety
- Lack of physical activity or poor fitness levels
- Dehydration or electrolyte imbalances
Making positive changes to these habits can often help reduce the frequency or severity of fast heart rate episodes.
Medical Conditions
Underlying health issues can also play a significant role in the development of a fast heart rate:
- High blood pressure
- Heart disease, including coronary artery disease and heart failure
- Thyroid disorders, such as hyperthyroidism
- Anemia or other blood-related conditions
- Infections or inflammation of the heart
Managing these conditions through medication, lifestyle changes, or other interventions can help address the underlying cause of the fast heart rate.
Medications and Substances
Certain medications and substances can increase the risk of developing a fast heart rate:
- Over-the-counter cold and cough medications containing stimulants
- Prescription medications for asthma or other respiratory conditions
- Illicit drugs, such as cocaine or amphetamines
If you suspect that a medication or substance is contributing to your fast heart rate, consult a healthcare professional for guidance on alternative options.
Treatments for a Fast Heart Rate
The treatment for a fast heart rate depends on the type, severity, and underlying cause of the condition. In some cases, lifestyle modifications may be sufficient, while others may require medical or surgical interventions.
Lifestyle Modifications
Making healthy lifestyle choices can significantly improve heart health and reduce the risk of a fast heart rate:
- Adopting a balanced diet rich in fruits, vegetables, and whole grains
- Engaging in regular physical activity, such as walking, swimming, or cycling
- Managing stress through relaxation techniques like yoga, meditation, or deep breathing exercises
- Avoiding excessive caffeine, alcohol, and tobacco use
- Maintaining a healthy weight and monitoring blood pressure regularly
Medications
Healthcare providers may prescribe medications to help control a fast heart rate and prevent complications:
- Beta-blockers to slow the heart rate and reduce the workload on the heart
- Calcium channel blockers to relax the heart muscle and improve blood flow
- Antiarrhythmic drugs to restore and maintain a normal heart rhythm
- Anticoagulants to reduce the risk of blood clots in individuals with atrial fibrillation
It is important to take medications as prescribed and report any side effects to your healthcare provider promptly.
Procedures and Surgeries
In cases where medications and lifestyle changes are insufficient, more advanced treatments may be necessary:
- Electrical cardioversion, which uses electric shocks to restore a normal heart rhythm
- Catheter ablation, a minimally invasive procedure that destroys small areas of heart tissue responsible for abnormal electrical signals
- Pacemaker implantation to regulate the heart’s rhythm
- Implantable cardioverter-defibrillator placement for individuals at risk of life-threatening arrhythmias
These procedures are typically performed by cardiologists or electrophysiologists and require careful evaluation to determine their suitability for each patient.
Emergency Interventions
In emergency situations, such as ventricular tachycardia or ventricular fibrillation, immediate action is required to stabilize the heart rhythm:
- Cardiopulmonary resuscitation to maintain blood flow during cardiac arrest
- Defibrillation to deliver an electric shock and restore a normal rhythm
- Administration of intravenous medications to stabilize the heart
Individuals with a history of severe arrhythmias may benefit from learning basic life support techniques or having access to automated external defibrillators.
When to Seek Medical Attention
While occasional episodes of a fast heart rate may not be cause for concern, certain symptoms warrant immediate medical attention:
- Chest pain or pressure
- Fainting or loss of consciousness
- Severe shortness of breath
- Rapid or irregular heartbeat accompanied by dizziness
- Persistent symptoms despite rest or self-care measures
Early diagnosis and treatment can help prevent complications and improve long-term outcomes for individuals with a fast heart rate.