Familial Mediterranean Fever, commonly abbreviated as FMF, is a rare genetic disorder that primarily affects people of Mediterranean descent. This condition is characterized by recurring episodes of fever and inflammation in various parts of the body, including the abdomen, chest, and joints. Understanding this illness requires a closer look at its causes, symptoms, diagnosis, treatment options, and the impact it has on patients’ lives.
Understanding the Causes
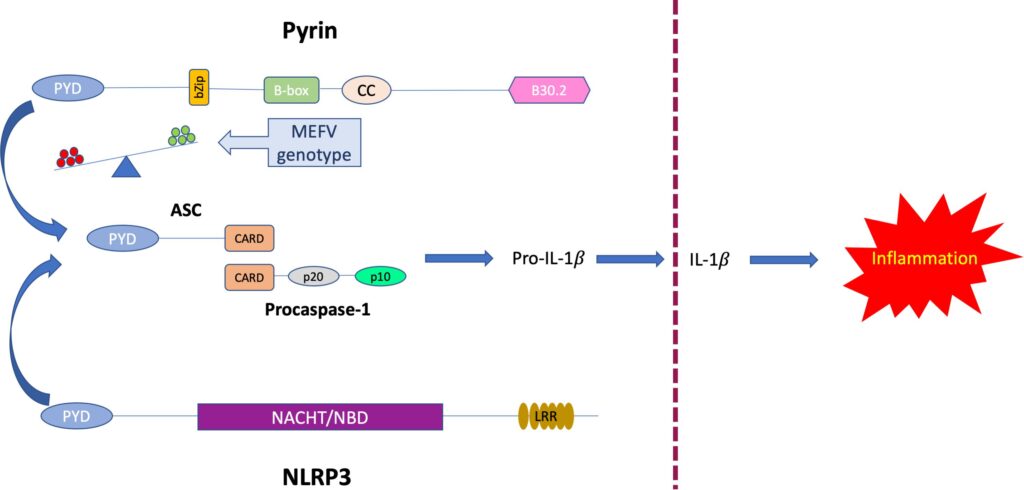
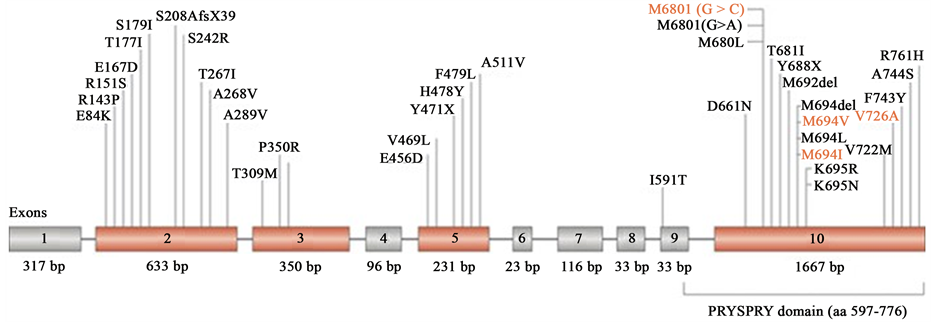
The root cause of this condition lies in mutations of a specific gene known as the MEFV gene. This gene provides instructions for making a protein called pyrin, which plays a crucial role in regulating inflammation within the body. When mutations occur in the MEFV gene, the resulting abnormal pyrin protein fails to control inflammation effectively, leading to the symptoms associated with the condition.
This illness follows an autosomal recessive inheritance pattern. This means that an individual must inherit two copies of the mutated gene—one from each parent—to develop the disease. People who inherit only one copy are carriers and typically do not show symptoms but can pass the mutation to their children.
Populations Most Affected
- Individuals of Armenian descent
- People from Arab communities
- Those of Jewish ancestry, particularly Sephardic and Mizrahi Jews
- Turkish populations
While these groups are more commonly affected, cases have also been reported in individuals from other ethnic backgrounds, highlighting the importance of awareness across diverse populations.
Symptoms and Their Impact
The hallmark of this condition is recurrent episodes of fever accompanied by inflammation. These episodes, often referred to as “attacks,” can vary in frequency, duration, and severity. Some individuals may experience attacks every few weeks, while others may go months without symptoms.
Common Symptoms During Attacks
- High fever, often lasting between one to three days
- Severe abdominal pain due to inflammation of the lining of the abdomen
- Chest pain caused by inflammation of the membrane surrounding the lungs
- Pain and swelling in the joints, most commonly affecting the knees, ankles, and hips
- Rashes, typically appearing as red, raised patches on the legs
Between attacks, individuals usually feel completely healthy, which can make the unpredictability of the condition particularly challenging. Over time, untreated or poorly managed cases can lead to complications such as amyloidosis, a serious condition where abnormal proteins build up in organs like the kidneys, potentially causing kidney failure.
Diagnosing the Condition
Diagnosing this illness can be complex due to the variability of symptoms and the lack of a definitive test. Physicians rely on a combination of clinical evaluation, family history, and laboratory tests to reach a diagnosis.
Clinical Evaluation
Doctors begin by taking a detailed medical history, paying close attention to patterns of fever and inflammation. They will ask about the frequency, duration, and triggers of attacks, as well as any family history of similar symptoms. Physical examinations during an attack may reveal tenderness in the abdomen, chest, or joints.
Laboratory Tests
Blood tests are often conducted to check for markers of inflammation, such as elevated levels of white blood cells and C-reactive protein. Genetic testing is another valuable tool, as it can identify mutations in the MEFV gene. However, not all individuals with the condition will have detectable mutations, so a negative genetic test does not rule out the diagnosis.
Diagnostic Criteria
To aid in diagnosis, healthcare providers often refer to established criteria, such as the Tel Hashomer criteria. These criteria consider factors like the presence of fever, location of pain, and response to specific medications. Meeting a certain number of criteria increases the likelihood of a correct diagnosis.
Treatment Options
While there is no cure for this condition, effective treatments are available to manage symptoms and prevent complications. The primary goal of treatment is to reduce the frequency and severity of attacks and to minimize the risk of long-term damage.
Medications
The cornerstone of treatment is a medication called colchicine. Colchicine works by reducing inflammation and preventing attacks when taken regularly. Most individuals respond well to this treatment, experiencing fewer and less severe episodes.
In cases where colchicine is not effective or tolerated, alternative medications such as biologic therapies may be prescribed. These include drugs like anakinra, canakinumab, and rilonacept, which target specific pathways involved in inflammation.
Importance of Adherence
Adhering to the prescribed treatment regimen is crucial. Skipping doses or discontinuing medication can increase the risk of attacks and complications. Patients are encouraged to work closely with their healthcare providers to find the most effective and manageable treatment plan.
Lifestyle Modifications
In addition to medication, certain lifestyle changes can help individuals better manage their condition:
- Maintaining a balanced diet to support overall health
- Staying hydrated, especially during attacks
- Avoiding known triggers, such as stress or excessive physical exertion
- Regular follow-ups with healthcare providers to monitor progress and adjust treatment as needed
Living with the Condition
Managing this illness requires a proactive approach to healthcare and a strong support system. Living with a chronic condition can be emotionally and physically taxing, but many individuals find ways to lead fulfilling lives with proper care.
Emotional and Psychological Impact
The unpredictable nature of attacks can lead to anxiety and stress. Some individuals may feel isolated or frustrated by the limitations imposed by their condition. Counseling and support groups can provide valuable emotional support and practical advice for coping with the challenges of living with this illness.
Impact on Daily Life
During an attack, individuals may need to take time off work or school to recover. Planning ahead and communicating openly with employers, teachers, and loved ones can help minimize disruptions. It is also important to have a plan in place for managing attacks when they occur, including access to necessary medications and emergency contacts.
Ongoing Research and Future Directions
Research into this condition continues to advance, offering hope for improved treatments and a deeper understanding of the underlying mechanisms. Scientists are exploring new medications, refining genetic testing methods, and investigating potential environmental factors that may influence the severity of symptoms.
Emerging Therapies
Recent studies have focused on targeting specific inflammatory pathways with precision medicine. These therapies aim to provide more personalized and effective treatment options for individuals who do not respond well to traditional medications.
Genetic Insights
Advances in genetic research are shedding light on why some individuals with mutations in the MEFV gene develop severe symptoms while others remain asymptomatic. This knowledge could pave the way for earlier diagnosis and tailored interventions based on an individual’s genetic profile.
Conclusion
Familial Mediterranean Fever remains a challenging but manageable condition for those affected. With ongoing advancements in medical science and increased awareness, individuals living with this illness can look forward to improved quality of life and better outcomes.