Factitious Disorder, often abbreviated as FD, is a complex mental health condition characterized by an individual’s deliberate fabrication or exaggeration of physical or psychological symptoms. This behavior is not driven by external rewards such as financial gain but rather by an internal need to assume the “sick role.” Understanding this disorder requires a closer look at its symptoms, underlying causes, and available treatment options.
Understanding Factitious Disorder
Factitious Disorder is a condition that falls under the broader category of somatic symptom and related disorders. Unlike malingering, where individuals fake illness for personal gain, those with this disorder are motivated by a deep-seated psychological need to be perceived as ill. The behavior often leads to unnecessary medical interventions, causing harm to the individual and straining healthcare resources.
Types of Factitious Disorder
- Factitious Disorder Imposed on Self: In this type, individuals intentionally produce or exaggerate symptoms in themselves. They may go to great lengths, such as self-inflicting injuries or tampering with medical tests, to convince others of their illness.
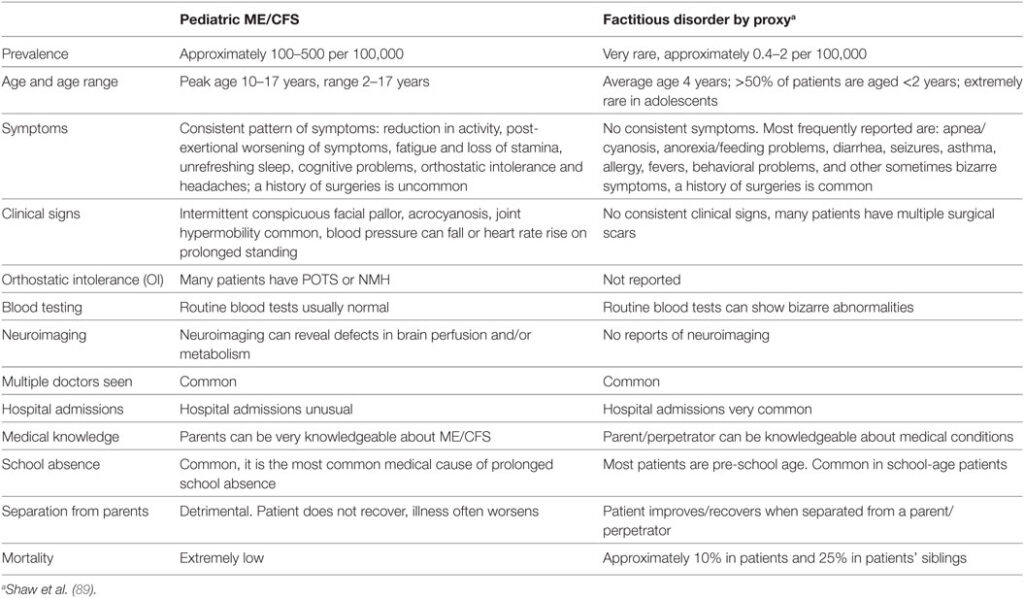
- Factitious Disorder Imposed on Another: Also known as Munchausen Syndrome by Proxy, this form involves a caregiver fabricating or inducing illness in another person, often a child or dependent. This variant is particularly concerning due to the potential for severe harm to the victim.
Symptoms of Factitious Disorder
The symptoms of this disorder can vary widely depending on the individual and the specific behaviors involved. However, some common signs include:
Physical Symptoms
- Frequent hospitalizations or visits to healthcare providers without a clear medical explanation.
- A detailed knowledge of medical terminology and procedures, often acquired through prior experiences in healthcare settings.
- Evidence of self-harm or tampering with medical equipment, such as injecting substances into veins or contaminating urine samples.
Psychological Symptoms
- An eagerness to undergo invasive or risky medical procedures, even when unnecessary.
- Inconsistent or contradictory medical history provided by the individual.
- A tendency to seek care from multiple healthcare providers or hospitals to avoid detection.
Behavioral Signs
- Resistance to allowing healthcare providers to communicate with family members or other doctors.
- Excessive enthusiasm for discussing medical details or participating in discussions about illnesses.
- A pattern of leaving healthcare facilities against medical advice when confronted or questioned.
Causes of Factitious Disorder
The exact cause of this disorder remains unclear, but several factors are believed to contribute to its development. These include:
Psychological Factors
Individuals with this disorder often have underlying emotional issues, such as low self-esteem, a need for attention, or unresolved trauma. Faking illness may serve as a coping mechanism to deal with feelings of inadequacy or loneliness. The act of being cared for by medical professionals can provide a sense of validation and control that they lack in other areas of life.
Environmental Influences
Growing up in an environment where illness was frequently emphasized or rewarded may predispose someone to develop this condition. For example, if a person received excessive attention or sympathy during childhood illnesses, they might unconsciously associate being sick with receiving love and care.
Biological Factors
Some researchers suggest that abnormalities in brain chemistry or functioning could play a role in the development of this disorder. While no definitive biological markers have been identified, studies continue to explore the potential links between neurological processes and factitious behaviors.
Treatment Options for Factitious Disorder
Treating this disorder is challenging because individuals often deny their behavior and resist seeking help. However, with a comprehensive approach involving mental health professionals, progress can be made. Below are some common treatment strategies:
Psychotherapy
Psychotherapy, particularly cognitive-behavioral therapy, is considered one of the most effective treatments for this disorder. It helps individuals recognize the motivations behind their behavior and develop healthier ways to cope with emotional distress. Therapists work closely with patients to address underlying issues such as trauma, anxiety, or depression.
Medication
While there are no medications specifically designed to treat this disorder, certain psychiatric drugs may be prescribed to manage co-occurring conditions like depression or anxiety. Antidepressants, anti-anxiety medications, or mood stabilizers can sometimes reduce the intensity of symptoms and improve overall functioning.
Hospital-Based Interventions
In cases where individuals pose a risk to themselves or others, hospitalization may be necessary. During these stays, healthcare teams focus on stabilizing the patient’s physical and mental health while addressing any immediate dangers posed by their actions. Long-term follow-up care is essential to prevent relapse.
Family Therapy
For cases involving Factitious Disorder Imposed on Another, family therapy is crucial. Caregivers who inflict harm on dependents require intensive intervention to break the cycle of abuse and protect the victim. Family members may also benefit from education about the disorder and guidance on how to support their loved one in recovery.
Support Groups
Joining support groups can provide individuals with a safe space to share their experiences and learn from others facing similar challenges. Peer support can foster a sense of community and accountability, encouraging participants to stay committed to their treatment plans.
Challenges in Diagnosis and Management
Diagnosing this disorder is notoriously difficult due to the deceptive nature of the condition. Individuals often go to great lengths to conceal their actions, making it hard for healthcare providers to identify the true problem. Additionally, many people with this disorder have extensive knowledge of medical systems, enabling them to manipulate situations effectively.
Ethical Dilemmas
Healthcare providers face ethical dilemmas when dealing with suspected cases of this disorder. On one hand, they must ensure that genuine medical conditions are not overlooked. On the other hand, they need to balance compassion with skepticism to avoid unnecessary interventions. Open communication among multidisciplinary teams is vital to navigating these complexities.
Patient Resistance
Many individuals with this disorder are reluctant to acknowledge their behavior, viewing it as integral to their identity. Convincing them to engage in treatment requires patience, empathy, and persistence. Building trust is key to breaking down barriers and encouraging cooperation.
Raising Awareness and Reducing Stigma
Public awareness of this disorder remains limited, leading to misunderstandings and stigma. Educating both healthcare professionals and the general public about the realities of this condition can promote early detection and more compassionate care. By fostering open conversations, society can create an environment where affected individuals feel comfortable seeking help.
Training for Healthcare Providers
Medical schools and training programs should incorporate modules on recognizing and managing this disorder. Equipping future healthcare workers with the skills to identify warning signs can improve outcomes and minimize harm to patients.
Community Education
Outreach initiatives aimed at raising awareness about this disorder can dispel myths and encourage individuals to seek assistance. Sharing stories of recovery and resilience can inspire hope and demonstrate that healing is possible.