Fabry Disease (FD) is a rare genetic disorder that affects multiple systems in the body. It is caused by mutations in the GLA gene, which leads to a deficiency in an enzyme called alpha-galactosidase A. This enzyme deficiency results in the accumulation of a specific type of fat, known as globotriaosylceramide, in various tissues and organs. Over time, this buildup can lead to severe complications affecting the kidneys, heart, brain, and other vital systems. In this article, we will explore the symptoms, diagnostic methods, and treatment options for Fabry Disease.
Understanding the Causes of Fabry Disease
Fabry Disease is an inherited condition that follows an X-linked recessive pattern. This means that the mutated gene responsible for the disease is located on the X chromosome. Males, who have only one X chromosome, are more severely affected because they lack a second X chromosome to compensate for the defective gene. Females, who have two X chromosomes, may experience milder symptoms or remain asymptomatic due to the presence of a healthy copy of the gene on their other X chromosome.
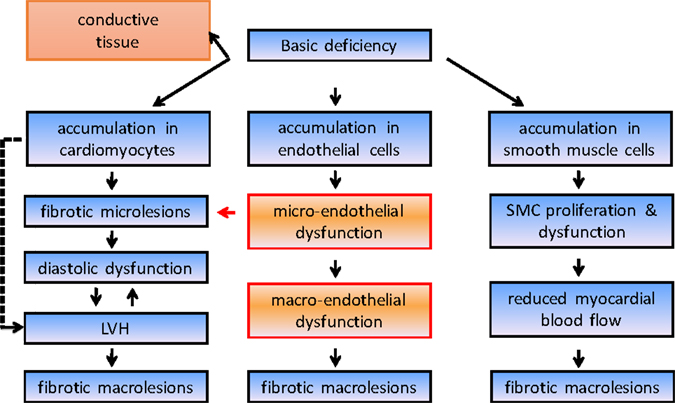
The primary cause of Fabry Disease is the deficiency of the enzyme alpha-galactosidase A. This enzyme plays a crucial role in breaking down globotriaosylceramide, a complex lipid found in the membranes of cells. When the enzyme is deficient or absent, globotriaosylceramide accumulates in the lysosomes of cells, leading to cellular dysfunction and damage. The progressive buildup of this substance is what causes the wide range of symptoms associated with the disease.
Symptoms of Fabry Disease
The symptoms of Fabry Disease vary widely among individuals and can manifest at different stages of life. They often appear in childhood but may not be recognized until later due to their nonspecific nature. Below are some of the most common symptoms associated with the disease:
Early Symptoms
- Pain and Burning Sensations: One of the hallmark symptoms of Fabry Disease is episodes of intense pain and burning sensations in the hands and feet, often referred to as acroparesthesia. These episodes can be triggered by factors such as heat, exercise, or stress.
- Rash-like Skin Lesions: Small, reddish-purple spots known as angiokeratomas may appear on the skin, particularly in areas like the groin, buttocks, and lower abdomen.
- Gastrointestinal Issues: Individuals with Fabry Disease often experience abdominal pain, diarrhea, nausea, and vomiting. These symptoms can mimic other gastrointestinal disorders, making diagnosis challenging.
Progressive Symptoms
- Kidney Problems: As the disease progresses, the accumulation of lipids in the kidneys can lead to proteinuria, reduced kidney function, and eventually kidney failure if left untreated.
- Heart Complications: Cardiac involvement is common in Fabry Disease and may include conditions such as left ventricular hypertrophy, arrhythmias, and heart failure.
- Neurological Manifestations: Some patients experience strokes, transient ischemic attacks, or hearing loss due to damage to blood vessels in the brain and ears.
Gender-Specific Differences
While males tend to exhibit more severe symptoms, females can also develop significant health issues related to Fabry Disease. However, the severity and onset of symptoms in females can vary greatly depending on the degree of X-chromosome inactivation, a process that determines which copy of the X chromosome is active in each cell.
Diagnosing Fabry Disease
Diagnosing Fabry Disease can be challenging due to its rarity and the overlap of its symptoms with those of other conditions. Early and accurate diagnosis is critical for initiating timely treatment and preventing irreversible organ damage. The following diagnostic methods are commonly used:
Clinical Evaluation
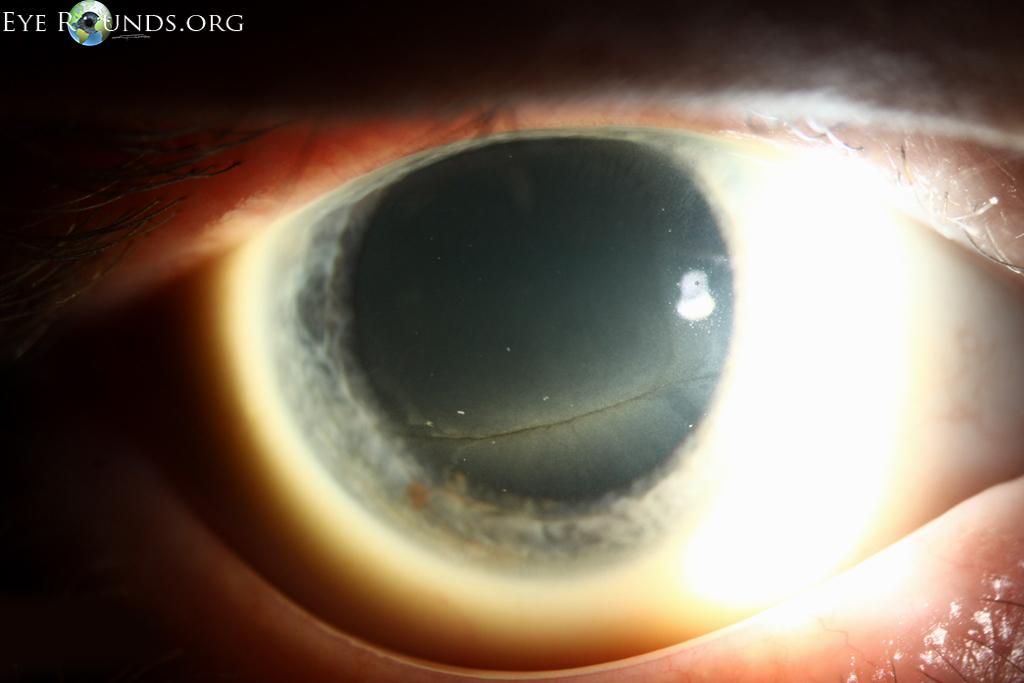
A thorough clinical evaluation is the first step in diagnosing Fabry Disease. Healthcare providers assess the patient’s medical history, family history, and symptoms. Special attention is paid to signs such as unexplained pain, skin lesions, and kidney or heart problems.
Enzyme Activity Testing
One of the key diagnostic tools for Fabry Disease is measuring the activity of the enzyme alpha-galactosidase A in the blood or tissues. Low or absent enzyme activity strongly suggests the presence of the disease. This test is particularly useful for diagnosing males, as they typically show significantly reduced enzyme levels.
Genetic Testing
Genetic testing is essential for confirming the diagnosis of Fabry Disease, especially in females. By analyzing the DNA for mutations in the GLA gene, healthcare providers can identify carriers and determine the specific genetic variant responsible for the disease.
Biomarker Analysis
In recent years, researchers have identified certain biomarkers, such as elevated levels of globotriaosylsphingosine in the blood or urine, that can aid in diagnosing Fabry Disease. These biomarkers provide additional evidence of the disease and help monitor its progression.
Treatment Options for Fabry Disease
Although there is no cure for Fabry Disease, several treatment options are available to manage symptoms, slow disease progression, and improve quality of life. These treatments focus on addressing both the underlying enzyme deficiency and the resulting complications.
Enzyme Replacement Therapy
Enzyme replacement therapy is a cornerstone of treatment for Fabry Disease. This approach involves administering synthetic versions of the missing enzyme intravenously to help break down accumulated lipids in the body. Two main types of enzyme replacement therapies are currently available:
- Agalsidase Alfa: This medication is derived from human cells and is administered every two weeks.
- Agalsidase Beta: Produced using recombinant technology, this treatment is also given every two weeks.
Enzyme replacement therapy has been shown to reduce lipid deposits in tissues, alleviate symptoms, and delay the progression of organ damage. However, it requires lifelong administration and may not completely reverse existing damage.
Chaperone Therapy
For some patients with specific mutations, chaperone therapy offers an alternative or complementary treatment option. Chaperone molecules work by stabilizing the defective enzyme and enhancing its activity. This approach is particularly beneficial for individuals with residual enzyme activity.
Symptomatic Treatments
In addition to addressing the root cause of Fabry Disease, managing symptoms is an important aspect of care. Medications and interventions may include:
- Pain Management: Anticonvulsants, antidepressants, and analgesics are often prescribed to alleviate chronic pain and discomfort.
- Kidney Support: Angiotensin-converting enzyme inhibitors or angiotensin receptor blockers may be used to protect kidney function and reduce proteinuria.
- Cardiac Care: Beta-blockers, antiarrhythmic drugs, and other cardiac medications help manage heart-related complications.
Lifestyle Modifications
Making lifestyle changes can also play a significant role in managing Fabry Disease. Patients are encouraged to adopt a healthy diet, engage in regular physical activity, avoid smoking, and limit alcohol consumption. These measures can help reduce the risk of cardiovascular and renal complications.
Regular Monitoring
Ongoing monitoring is essential for individuals with Fabry Disease to track disease progression and adjust treatment plans as needed. Regular assessments of kidney function, heart health, and neurological status ensure early detection of complications and prompt intervention.
Emerging Therapies and Research
Research into new therapies for Fabry Disease is ongoing, offering hope for improved outcomes in the future. Gene therapy, for example, aims to correct the underlying genetic defect by introducing functional copies of the GLA gene into the body. While still in experimental stages, this approach holds promise for providing a long-term solution to the enzyme deficiency.
Other investigational treatments include substrate reduction therapy, which works by decreasing the production of the lipid that accumulates in Fabry Disease, and novel chaperone molecules designed to target a broader range of mutations. Clinical trials are underway to evaluate the safety and efficacy of these innovative approaches.
Collaborative efforts between researchers, healthcare providers, and patient advocacy groups continue to drive advancements in understanding and treating Fabry Disease. Increased awareness and funding for research are critical to improving diagnostic tools, expanding treatment options, and ultimately finding a cure.