Epilepsy is a neurological condition that affects millions of people worldwide. Abbreviated as “Epi,” it is characterized by recurring seizures caused by abnormal electrical activity in the brain. This article explores the different types of epilepsy, common triggers that can lead to seizures, and the available treatment options for managing this condition.
Understanding Epilepsy
Epilepsy is not a single disease but rather a spectrum of disorders involving the central nervous system. It is marked by unpredictable seizures, which are episodes of disturbed brain activity that can affect behavior, movement, or consciousness. The severity and frequency of seizures vary from person to person, making epilepsy a highly individualized condition.
How Epilepsy Affects the Brain
The human brain functions through a complex network of neurons that communicate via electrical signals. In individuals with epilepsy, these signals become disrupted, leading to sudden bursts of electrical activity. These bursts can interfere with normal brain function, resulting in seizures. Seizures can manifest in various ways, such as convulsions, staring spells, or brief periods of confusion.
Types of Epilepsy
There are several types of epilepsy, each classified based on the type of seizure experienced and the part of the brain affected. Understanding these types is crucial for proper diagnosis and treatment.
Focal Epilepsy
Focal epilepsy occurs when seizures originate in a specific area of the brain. These seizures may be further categorized into two subtypes:
- Focal Aware Seizures: Previously known as simple partial seizures, these occur when the individual remains conscious during the episode. Symptoms may include unusual sensations, emotional changes, or involuntary movements in one part of the body.
- Focal Impaired Awareness Seizures: Formerly called complex partial seizures, these involve a loss of awareness or consciousness. During these episodes, the person may exhibit repetitive behaviors, such as lip-smacking or wandering aimlessly.
Generalized Epilepsy
Generalized epilepsy involves seizures that affect both hemispheres of the brain simultaneously. There are several subtypes of generalized seizures:
- Absence Seizures: Often seen in children, absence seizures cause brief lapses in attention. The person may appear to be staring blankly into space for a few seconds.
- Tonic-Clonic Seizures: These are the most widely recognized type of seizure and involve two phases. The tonic phase causes muscle stiffening, while the clonic phase leads to rhythmic jerking movements.
- Myoclonic Seizures: These seizures result in sudden, brief muscle jerks, often affecting the arms or legs.
- Atonic Seizures: Also known as drop seizures, these cause a sudden loss of muscle tone, leading to falls or head drops.
Unknown Onset Epilepsy
In some cases, the origin of the seizure cannot be determined. This category, known as unknown onset epilepsy, includes seizures where the initial symptoms are unclear or where diagnostic tools fail to pinpoint the exact location of abnormal brain activity.
Common Triggers for Seizures
While seizures can occur spontaneously, certain factors are known to trigger them. Identifying and avoiding these triggers can help reduce the frequency of episodes.
Sleep Deprivation
Lack of sleep is one of the most common seizure triggers. Sleep deprivation disrupts the brain’s natural rhythm, increasing the likelihood of abnormal electrical activity. Maintaining a consistent sleep schedule and ensuring adequate rest can significantly lower the risk of seizures.
Stress
Stress has a profound impact on the brain and can exacerbate epilepsy symptoms. Chronic stress alters hormone levels and neurotransmitter activity, making the brain more susceptible to seizures. Techniques such as mindfulness, meditation, and therapy can help manage stress effectively.
Flashing Lights
Some individuals with epilepsy are sensitive to flashing lights or patterns, a phenomenon known as photosensitivity. Exposure to strobe lights, video games, or even sunlight flickering through trees can trigger seizures in susceptible individuals. Wearing specialized glasses or avoiding triggering stimuli can mitigate this risk.
Alcohol and Drug Use
Substance abuse, including excessive alcohol consumption and recreational drug use, can increase the likelihood of seizures. Alcohol withdrawal, in particular, is a well-known trigger for seizures in individuals with epilepsy. Seeking professional help for substance abuse can improve overall health and reduce seizure frequency.
Hormonal Changes
Hormonal fluctuations, especially in women, can influence seizure activity. Menstrual cycles, pregnancy, and menopause may alter the balance of hormones in the body, potentially triggering seizures. Working closely with healthcare providers to manage hormonal changes can be beneficial.
Treatment Options for Epilepsy
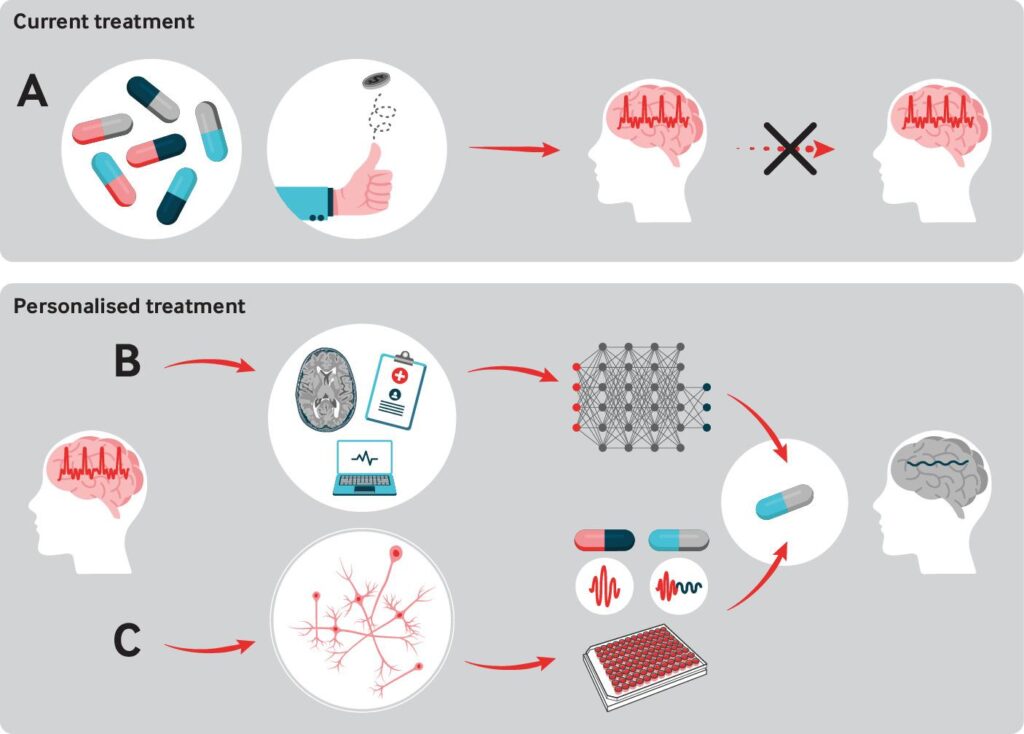
While there is no cure for epilepsy, various treatment options are available to manage symptoms and improve quality of life. The choice of treatment depends on the type of epilepsy, the frequency of seizures, and the individual’s overall health.
Medication
Anti-seizure medications are the most common form of treatment for epilepsy. These drugs work by stabilizing electrical activity in the brain, thereby reducing the frequency and severity of seizures. Some commonly prescribed medications include:
- Carbamazepine
- Valproate
- Lamotrigine
- Levetiracetam
It is important to note that finding the right medication and dosage may require trial and error. Regular follow-ups with a healthcare provider are essential to monitor effectiveness and manage side effects.
Surgery
For individuals whose seizures cannot be controlled with medication, surgery may be an option. Surgical procedures aim to remove or isolate the part of the brain responsible for seizures. Common surgical interventions include:
- Resective Surgery: Involves removing the portion of the brain where seizures originate.
- Vagus Nerve Stimulation: Implants a device that sends electrical impulses to the brain via the vagus nerve, helping to reduce seizure frequency.
- Responsive Neurostimulation: Uses a device implanted in the skull to detect and respond to abnormal brain activity.
Dietary Therapies
Certain dietary approaches have shown promise in managing epilepsy, particularly in children. The ketogenic diet, which is high in fats and low in carbohydrates, has been effective in reducing seizures in some individuals. Another option is the modified Atkins diet, which is less restrictive but still emphasizes high-fat intake.
Alternative Therapies
In addition to conventional treatments, some individuals explore alternative therapies to complement their care. These may include:
- Acupuncture: Involves inserting thin needles into specific points on the body to promote relaxation and balance.
- Biofeedback: Teaches individuals to control physiological processes, such as heart rate and muscle tension, to reduce seizure activity.
- Herbal Supplements: Certain herbs, such as valerian root and passionflower, are believed to have calming effects, though their efficacy is not scientifically proven.
Supportive Care
Beyond medical interventions, supportive care plays a vital role in managing epilepsy. This includes:
- Education: Learning about epilepsy empowers individuals and their families to make informed decisions about treatment and lifestyle choices.
- Support Groups: Connecting with others who have epilepsy can provide emotional support and practical advice.
- Safety Measures: Implementing safety precautions, such as wearing protective helmets or using seizure alarms, can prevent injuries during episodes.
Living with Epilepsy
Managing epilepsy requires a comprehensive approach that addresses both physical and emotional needs. By understanding the types of epilepsy, recognizing potential triggers, and exploring available treatments, individuals can take proactive steps toward living a fulfilling life despite the challenges posed by this condition.