Epidermolysis Bullosa, commonly abbreviated as EB, is a group of rare genetic conditions that affect the skin and mucous membranes. These disorders are characterized by fragile skin that blisters and tears easily, often leading to significant physical and emotional challenges for those affected. While Epidermolysis Bullosa is not widely known, understanding its causes, symptoms, types, and available treatments is crucial for improving the quality of life for patients and their families.
What is Epidermolysis Bullosa?
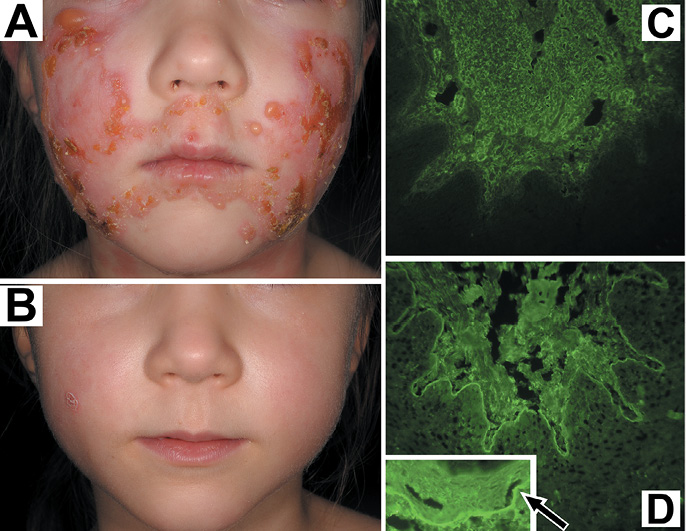
Epidermolysis Bullosa refers to a collection of inherited disorders that cause the skin to be extraordinarily fragile. Even minor friction or trauma can result in painful blisters and open wounds. The condition affects both children and adults, though it is typically present at birth or develops shortly thereafter. The severity of the disorder varies depending on the specific type and subtype, but all forms share the hallmark feature of blistering skin.
The Science Behind the Disorder
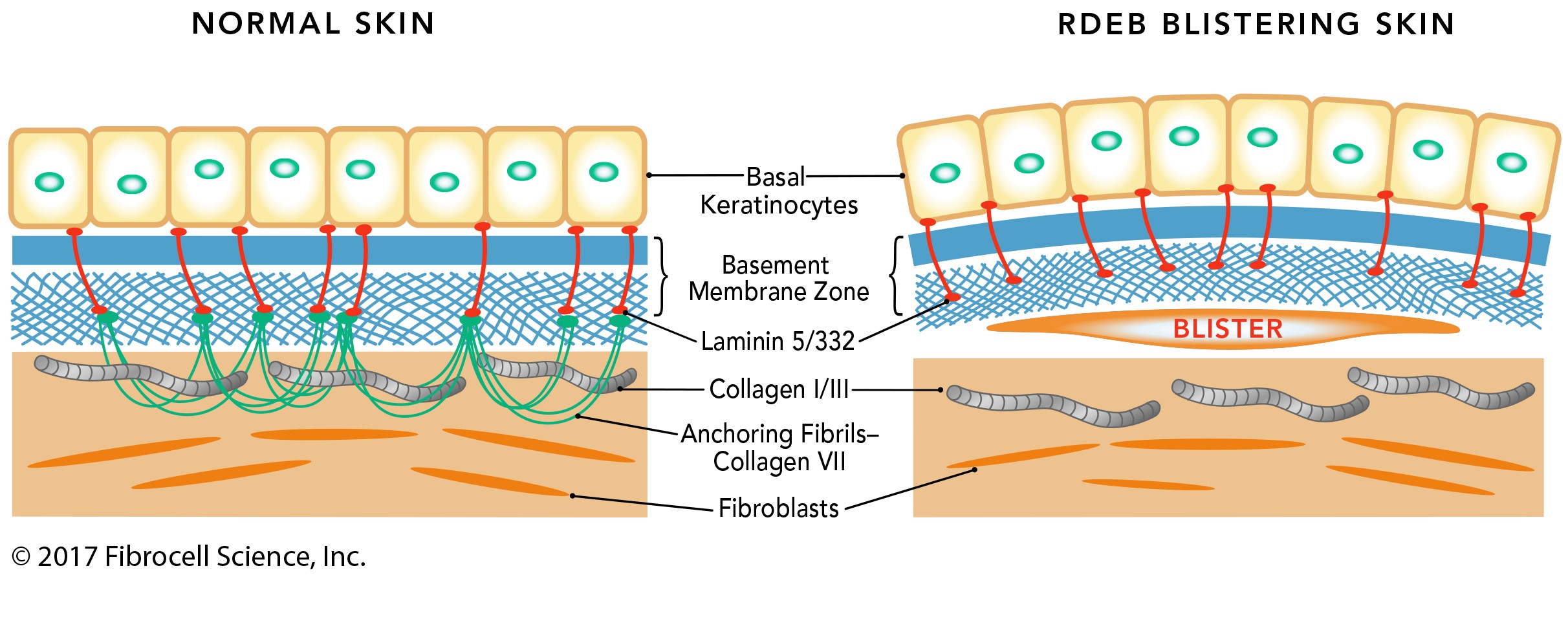
At its core, this condition arises due to genetic mutations that impair the proteins responsible for anchoring the layers of the skin together. In healthy individuals, these proteins ensure that the outer layer of the skin, called the epidermis, remains securely attached to the underlying layer, known as the dermis. When these proteins are defective or missing, the skin becomes highly susceptible to separation, resulting in blisters and erosions.
Types of Epidermolysis Bullosa
There are several distinct types of this rare skin disorder, each classified based on the specific layer of the skin where blistering occurs. Understanding these categories is essential for diagnosing and managing the condition effectively.
Epidermolysis Bullosa Simplex
- Overview: This is the most common and usually the mildest form of the condition. Blisters form in the epidermis, the outermost layer of the skin.
- Symptoms: Patients may experience blisters primarily on the hands and feet, which tend to heal without scarring. However, some subtypes can lead to more widespread blistering.
- Cause: Mutations in genes such as KRT5 and KRT14, which encode keratin proteins, are responsible for this type.
Junctional Epidermolysis Bullosa
- Overview: This form is more severe and involves blistering within the lamina lucida, a part of the basement membrane zone between the epidermis and dermis.
- Symptoms: Blisters often appear at birth or shortly after and can affect internal organs and mucous membranes, such as the mouth and esophagus.
- Cause: Defects in genes like LAMA3, LAMB3, and COL17A1 disrupt the structural integrity of the skin.
Dystrophic Epidermolysis Bullosa
- Overview: This type is characterized by blistering below the basement membrane, in the upper part of the dermis.
- Symptoms: Blisters often heal with significant scarring, which can lead to deformities such as fused fingers and toes. Severe cases may involve extensive scarring and an increased risk of skin cancer.
- Cause: Mutations in the COL7A1 gene, which encodes collagen VII, are responsible for this form.
Kindler Syndrome
- Overview: This is a mixed type of the disorder, where blistering can occur in multiple layers of the skin.
- Symptoms: In addition to fragile skin, patients may experience photosensitivity, progressive poikiloderma (skin discoloration), and mucosal involvement.
- Cause: Mutations in the FERMT1 gene contribute to this rare subtype.
Symptoms and Complications
The symptoms of this rare skin disorder vary widely depending on the type and severity of the condition. However, there are common features that many patients experience.
Common Symptoms
- Blisters on the skin, especially in areas prone to friction such as the hands, feet, knees, and elbows.
- Open wounds that are slow to heal and prone to infection.
- Scarring, which can lead to deformities such as contractures (tightening of the skin) and fusion of fingers or toes.
- Thickened nails or loss of nails.
- Mucosal involvement, including blistering in the mouth, throat, and gastrointestinal tract, leading to difficulty eating and swallowing.
Potential Complications
In addition to the immediate symptoms, individuals with this condition face a range of long-term complications that can significantly impact their health and well-being.
- Infections: Open wounds are highly susceptible to bacterial infections, which can become systemic and life-threatening if not treated promptly.
- Nutritional Challenges: Blistering in the mouth and esophagus can make eating painful, leading to malnutrition and poor growth, particularly in children.
- Skin Cancer: Certain forms of the disorder increase the risk of developing aggressive forms of skin cancer, such as squamous cell carcinoma.
- Psychological Impact: Chronic pain, disfigurement, and social isolation can contribute to anxiety, depression, and other mental health challenges.
Diagnosis and Testing
Early and accurate diagnosis is critical for managing this rare skin disorder effectively. Several methods are used to identify the condition and determine its specific type.
Clinical Evaluation
A thorough physical examination is often the first step in diagnosing the disorder. Doctors look for characteristic signs such as blistering, scarring, and nail abnormalities. A detailed family history is also essential, as the condition is inherited.
Genetic Testing
Genetic testing plays a pivotal role in confirming the diagnosis and identifying the specific mutation responsible for the disorder. This information is invaluable for understanding the prognosis and guiding treatment decisions.
Skin Biopsy
In some cases, a skin biopsy may be performed. During this procedure, a small sample of skin is removed and examined under a microscope to determine the layer where blistering occurs. This helps classify the type of the disorder.
Treatment and Management
While there is currently no cure for this rare skin disorder, various treatments and strategies can help manage symptoms, prevent complications, and improve quality of life.
Wound Care
Proper wound care is a cornerstone of managing the condition. This includes:
- Regularly cleaning and dressing blisters and wounds to prevent infection.
- Using non-adhesive dressings to minimize further damage to the skin.
- Applying topical medications to promote healing and reduce pain.
Pain Management
Chronic pain is a common challenge for individuals with this condition. Pain management strategies may include:
- Over-the-counter or prescription pain relievers.
- Physical therapy to address joint stiffness and improve mobility.
- Psychological support to help cope with chronic discomfort.
Nutritional Support
For patients with oral or esophageal involvement, nutritional support is crucial. This may involve:
- Working with a dietitian to develop a balanced meal plan.
- Using nutritional supplements or feeding tubes in severe cases.
- Addressing any underlying gastrointestinal issues.
Emerging Therapies
Research into new treatments is ongoing, offering hope for improved outcomes in the future. Some promising approaches include:
- Gene therapy to correct the underlying genetic mutations.
- Stem cell transplantation to regenerate healthy skin tissue.
- Topical and systemic medications targeting inflammation and wound healing.
Living with the Condition
Living with this rare skin disorder presents unique challenges, but with proper care and support, individuals can lead fulfilling lives. Education, advocacy, and community resources play a vital role in empowering patients and their families.
Support Networks
Connecting with others who understand the challenges of living with this condition can provide emotional support and practical advice. Support groups, both online and in-person, offer a platform for sharing experiences and coping strategies.
Educational Resources
Access to reliable information about the condition is essential for making informed decisions about care. Organizations dedicated to raising awareness and funding research can be valuable sources of knowledge and assistance.
Advocacy and Awareness
Raising awareness about this rare skin disorder is critical for reducing stigma and promoting understanding. Advocacy efforts can also drive policy changes and increase funding for research into new treatments.