An epidermal cyst, often mistakenly referred to as a sebaceous cyst, is a common skin condition that many people encounter at some point in their lives. These cysts are small, round lumps that form beneath the skin and are usually harmless. However, they can sometimes cause discomfort or become infected, requiring medical attention. In this article, we will explore the details of epidermal cysts, including their causes, how they are diagnosed, and the available treatment options.
What Is an Epidermal Cyst?
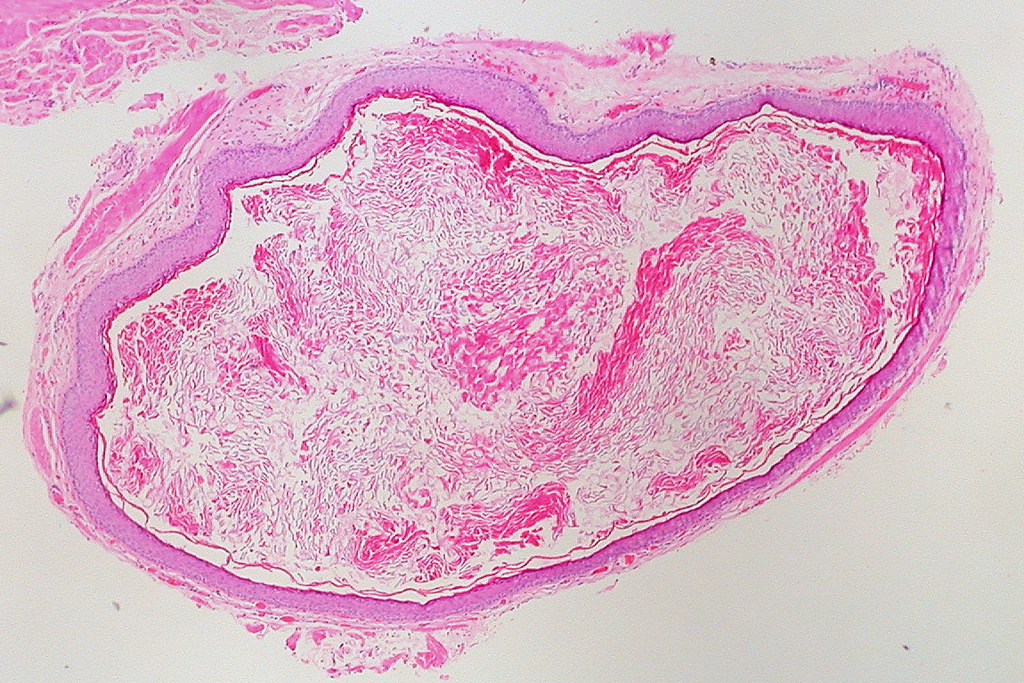
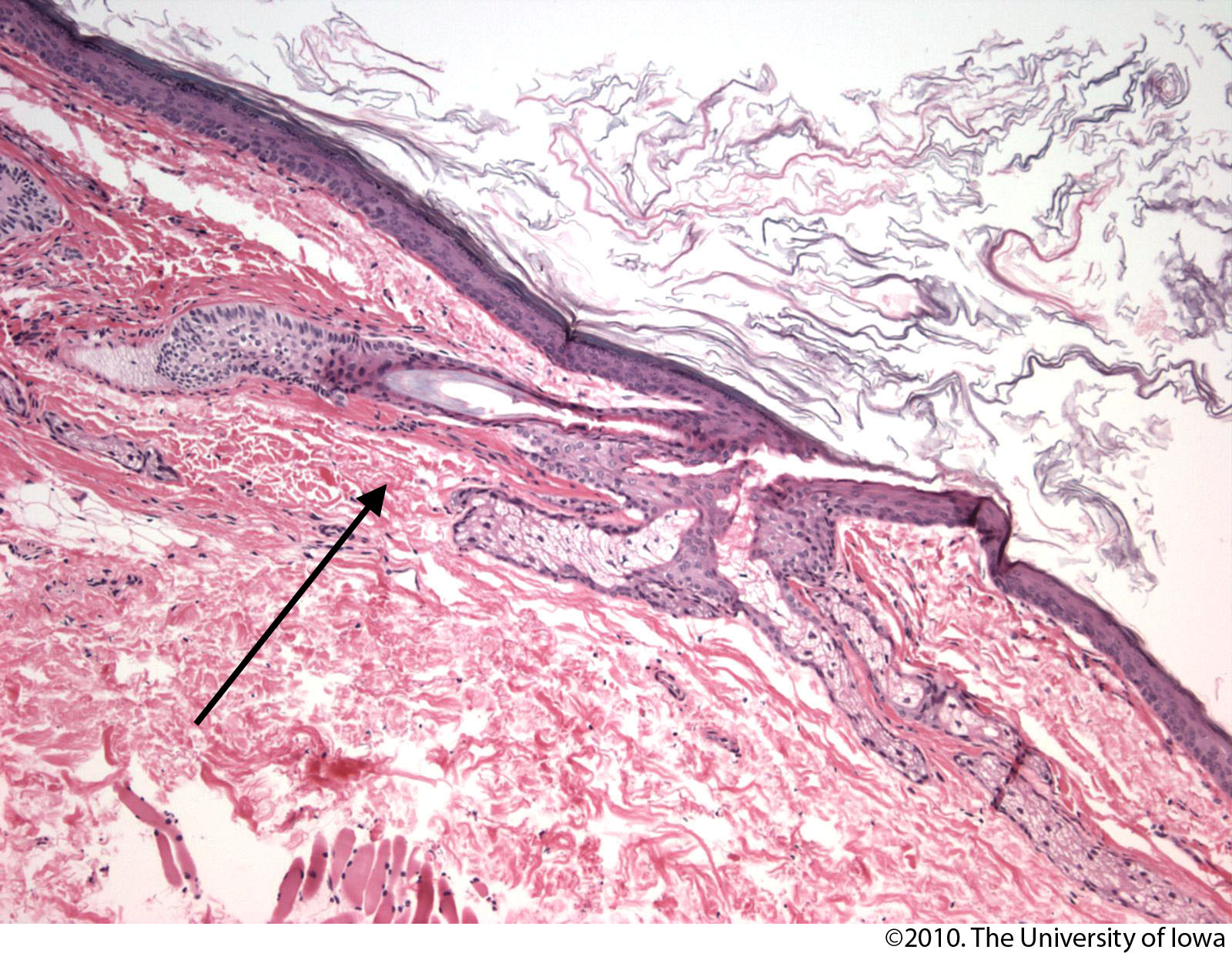
An epidermal cyst is a closed sac-like structure that forms under the skin. It is filled with keratin, a protein found in hair, skin, and nails. These cysts typically develop slowly and are most commonly found on areas of the body such as the face, neck, chest, and back. Despite being called “sebaceous cysts” by some, they do not originate from sebaceous glands but rather from the epidermis, which is the outermost layer of the skin.
Characteristics of Epidermal Cysts
- They are usually round and dome-shaped.
- The size can range from a few millimeters to several centimeters in diameter.
- They are often movable and feel firm or slightly soft to the touch.
- In some cases, they may have a small opening in the center where keratin can be discharged.
Causes of Epidermal Cysts
Understanding the causes of epidermal cysts can help individuals take preventive measures and recognize potential risk factors. While these cysts are generally benign, certain conditions and behaviors can contribute to their formation.
Blocked Hair Follicles
One of the primary causes of epidermal cysts is the blockage of hair follicles. Hair follicles are tiny structures in the skin where hair grows. When these follicles become blocked due to dirt, oil, or dead skin cells, it can lead to the formation of a cyst. This blockage traps keratin inside the follicle, causing it to accumulate and form a cyst.
Trauma or Injury to the Skin
Physical trauma or injury to the skin can also result in the development of epidermal cysts. When the skin is damaged, the healing process may cause cells to multiply abnormally, leading to the formation of a cyst. This is particularly common in areas of the body that are frequently exposed to friction or pressure.
Hormonal Changes
Hormonal fluctuations, especially during puberty, pregnancy, or menopause, can increase the likelihood of developing epidermal cysts. Hormones play a significant role in regulating the production of sebum, an oily substance that lubricates the skin. Excessive sebum production can clog pores and contribute to cyst formation.
Genetic Factors
Some individuals may be genetically predisposed to developing epidermal cysts. Certain inherited conditions, such as Gardner’s syndrome or basal cell nevus syndrome, are associated with an increased risk of cyst formation. If you have a family history of epidermal cysts, you may be more likely to experience them yourself.
Diagnosing Epidermal Cysts
Diagnosing an epidermal cyst is usually straightforward, but in some cases, further evaluation may be necessary to rule out other conditions. Healthcare providers rely on a combination of physical examination, patient history, and diagnostic tests to confirm the presence of a cyst.
Physical Examination
A healthcare provider will begin by examining the cyst visually and palpating it to assess its size, shape, and texture. Epidermal cysts are typically smooth, round, and movable under the skin. The provider may also inquire about any symptoms, such as pain, redness, or discharge, which could indicate infection or inflammation.
Medical History
Understanding the patient’s medical history is crucial for accurate diagnosis. The healthcare provider may ask questions about when the cyst first appeared, whether it has changed in size or appearance, and if there is a history of similar growths in the family. This information helps differentiate epidermal cysts from other types of skin lesions.
Diagnostic Tests
In rare cases where the diagnosis is uncertain, additional tests may be required. These tests can include:
- Ultrasound: This imaging technique uses sound waves to create a picture of the cyst, helping to determine its depth and contents.
- Biopsy: A small sample of tissue may be removed and examined under a microscope to confirm the diagnosis and rule out other conditions, such as cancerous growths.
Treatment Options for Epidermal Cysts
While many epidermal cysts do not require treatment and may resolve on their own, others may need medical intervention. The choice of treatment depends on factors such as the size of the cyst, its location, and whether it is causing discomfort or infection.
Observation and Monitoring
For small, asymptomatic cysts, healthcare providers often recommend a “watch and wait” approach. Regular monitoring ensures that the cyst does not grow or become problematic. During this time, patients are advised to avoid squeezing or irritating the cyst, as this can lead to infection or scarring.
Warm Compresses
Applying warm compresses to the cyst can help reduce inflammation and promote drainage. This simple home remedy involves soaking a clean cloth in warm water and placing it over the cyst for 10 to 15 minutes several times a day. Warm compresses are particularly effective for cysts that are tender or inflamed.
Incision and Drainage
If the cyst becomes infected or painful, a healthcare provider may perform a minor procedure called incision and drainage. This involves making a small cut in the cyst to remove its contents. While this provides immediate relief, it does not prevent the cyst from recurring, as the sac remains intact.
Surgical Excision
For persistent or recurrent cysts, surgical excision is often the most effective treatment. This procedure involves removing the entire cyst, including its sac, to prevent regrowth. Surgical excision is typically performed under local anesthesia and may leave a small scar. However, the benefits of complete removal often outweigh the cosmetic concerns.
Antibiotics
If the cyst becomes infected, antibiotics may be prescribed to treat the infection. Oral or topical antibiotics can help reduce inflammation and eliminate bacteria. However, antibiotics alone cannot cure the cyst, and additional treatment may be necessary once the infection is under control.
Preventing Epidermal Cysts
While it may not always be possible to prevent epidermal cysts, certain practices can reduce the risk of their formation. Maintaining good skin hygiene, avoiding excessive sun exposure, and protecting the skin from injury are all effective preventive measures.
Proper Skincare
Regular cleansing and exfoliation can help prevent the buildup of dead skin cells and oils that contribute to cyst formation. Using non-comedogenic skincare products that do not clog pores is also recommended.
Avoiding Skin Trauma
Protecting the skin from cuts, scrapes, and burns can minimize the risk of cyst development. Wearing protective clothing and using sunscreen can shield the skin from environmental damage.
Managing Hormonal Changes
For individuals prone to hormonal fluctuations, managing these changes through lifestyle modifications or medical treatment may help reduce the likelihood of cysts. A balanced diet, regular exercise, and stress management can all contribute to hormonal balance.
When to Seek Medical Attention
While most epidermal cysts are harmless, certain signs and symptoms warrant prompt medical attention. These include:
- Rapid growth or significant enlargement of the cyst.
- Persistent pain, redness, or swelling around the cyst.
- Discharge of pus or foul-smelling material from the cyst.
- Fever or other systemic symptoms accompanying the cyst.
If any of these symptoms occur, it is important to consult a healthcare provider to rule out infection or other underlying conditions.