Eosinophilic Esophagitis, commonly abbreviated as EoE, is a chronic immune-mediated condition that affects the esophagus. This disorder occurs when a specific type of white blood cell, known as eosinophils, accumulates in the lining of the esophagus. The presence of these cells leads to inflammation and damage, causing a range of symptoms that can significantly impact a person’s quality of life. In this article, we will explore the underlying causes, common symptoms, diagnostic methods, and available treatment options for this increasingly recognized condition.
Understanding the Causes
The exact cause of this condition remains unclear, but researchers believe it results from a combination of genetic, environmental, and immune system factors. Below are some key contributors:
Allergic Reactions
- Many individuals with this condition also suffer from other allergic disorders, such as asthma, eczema, or food allergies. This suggests a link between allergic reactions and the development of the disease.
- Certain foods, including dairy products, wheat, eggs, soy, nuts, and seafood, are often identified as triggers. However, the specific food allergens responsible can vary from person to person.
Environmental Factors
- Airborne allergens like pollen, dust mites, and animal dander may contribute to the condition, particularly in individuals who are genetically predisposed.
- Seasonal variations in symptoms have been observed, further supporting the role of environmental triggers.
Immune System Dysfunction
- In people with this condition, the immune system mistakenly identifies harmless substances, such as food proteins, as threats. This leads to an overproduction of eosinophils in the esophagus.
- Genetic factors may play a role in making some individuals more susceptible to immune system dysfunction.
Recognizing the Symptoms
Symptoms of this condition can vary depending on the age of the individual. Children and adults often experience different manifestations, which can sometimes make diagnosis challenging.
Symptoms in Children
- Difficulty swallowing, which may lead to refusal to eat or poor weight gain.
- Vomiting or regurgitation, especially after meals.
- Abdominal pain or discomfort.
- Frequent episodes of choking on food.
Symptoms in Adults
- Trouble swallowing solid foods, often described as a sensation of food getting stuck in the throat.
- Chest pain that is not related to heart issues.
- Heartburn-like symptoms that do not improve with standard acid reflux treatments.
- Food impaction, where food becomes lodged in the esophagus and requires medical intervention to remove.
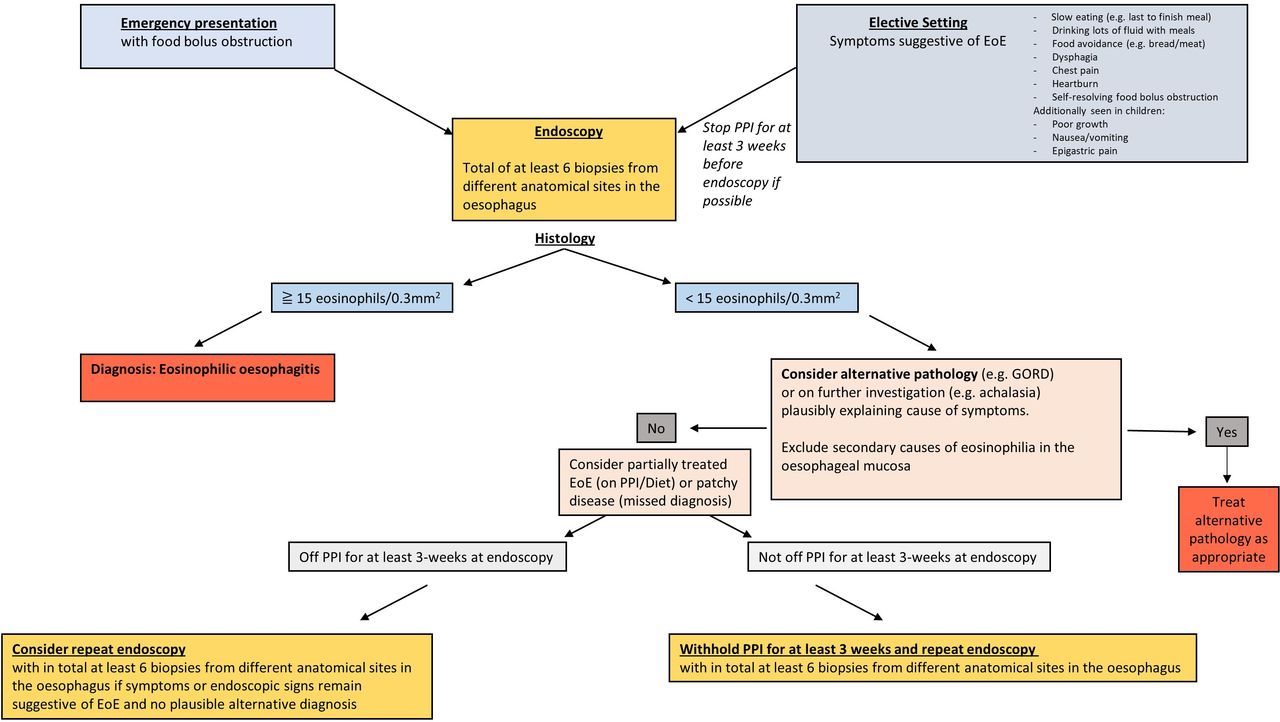
Diagnostic Process
Diagnosing this condition involves a combination of clinical evaluation, imaging studies, and specialized tests. Because its symptoms overlap with other gastrointestinal disorders, a thorough diagnostic approach is essential.
Medical History and Physical Examination
- A healthcare provider will begin by taking a detailed medical history, paying close attention to symptoms, dietary habits, and any history of allergies.
- A physical examination may reveal signs such as malnutrition or growth delays in children, which can indicate long-standing issues with eating.
Endoscopy and Biopsy
- An endoscopy is a procedure where a thin, flexible tube with a camera is inserted into the esophagus to examine its lining. During this procedure, the doctor may observe characteristic signs such as rings, narrow areas, or white spots caused by eosinophil accumulation.
- Biopsies, or small tissue samples, are taken during the endoscopy and examined under a microscope. A high concentration of eosinophils in the esophageal tissue confirms the diagnosis.
Elimination Diet and Allergy Testing
- To identify potential food triggers, doctors may recommend an elimination diet. This involves removing common allergenic foods from the diet and gradually reintroducing them while monitoring symptoms.
- Allergy testing, such as skin prick tests or blood tests, can help pinpoint specific allergens contributing to the condition.
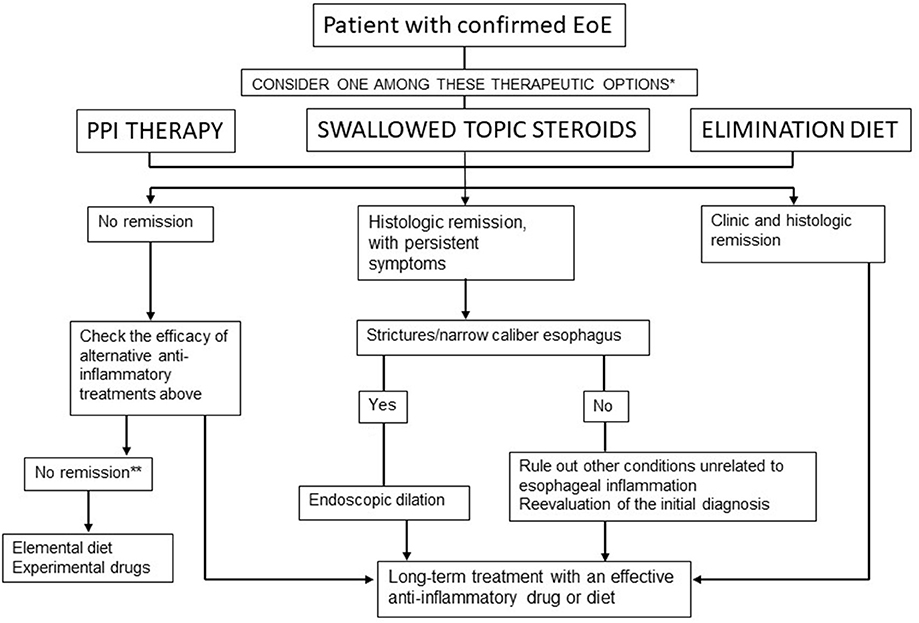
Treatment Options
While there is no cure for this condition, several treatment strategies can effectively manage symptoms and improve quality of life. These approaches focus on reducing inflammation, addressing underlying triggers, and preventing complications.
Dietary Management
- One of the most effective ways to manage this condition is through dietary changes. An elimination diet, as mentioned earlier, can help identify and avoid trigger foods.
- In some cases, a specialized dietitian may recommend an elemental diet, which involves consuming nutritionally complete formulas that are free of allergenic proteins.
Medications
- Proton pump inhibitors, commonly used to treat acid reflux, can sometimes reduce inflammation in the esophagus and alleviate symptoms.
- Topical corticosteroids, administered in the form of swallowed asthma inhalers or liquid preparations, are often prescribed to reduce eosinophil levels and control inflammation.
Dilation Procedures
- For individuals with severe narrowing of the esophagus, a procedure called esophageal dilation may be necessary. This involves stretching the esophagus to improve swallowing.
- Dilation is typically reserved for cases where dietary and medication interventions have not been sufficient.
Lifestyle Modifications
- Avoiding known allergens, both dietary and environmental, can help prevent symptom flare-ups.
- Eating smaller, more frequent meals and chewing food thoroughly can reduce the risk of food impaction.
- Managing stress and maintaining a healthy lifestyle can also support overall digestive health.
Ongoing Research and Emerging Treatments
Researchers continue to investigate new therapies and treatment options for this condition. Some promising areas of research include:
- Biologic Therapies: Medications that target specific components of the immune system are being studied for their potential to reduce eosinophil activity in the esophagus.
- Genetic Studies: Understanding the genetic basis of the condition may lead to personalized treatment approaches in the future.
- Improved Diagnostic Tools: Advances in imaging and biomarker identification could enhance early detection and monitoring of the disease.
By staying informed about the latest developments, patients and healthcare providers can work together to optimize management strategies and improve outcomes.