An endometrial polyp, often referred to as a uterine polyp, is a growth that forms on the inner lining of the uterus, known as the endometrium. These growths are usually benign but can sometimes lead to complications such as abnormal bleeding or fertility issues. Understanding this condition is essential for women who may experience symptoms or are concerned about their reproductive health. In this article, we will explore what endometrial polyps are, their potential causes, how they are diagnosed, and the available treatment options.

What Are Endometrial Polyps?
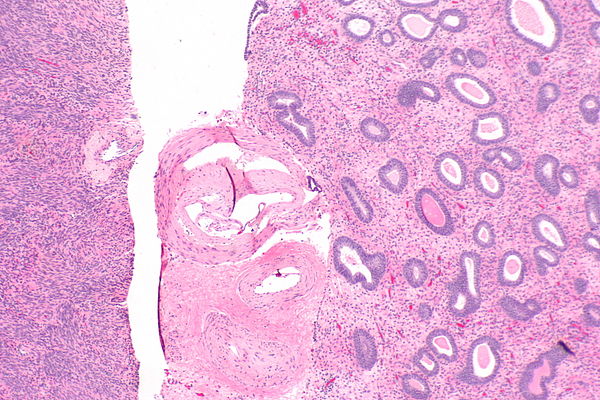
Endometrial polyps are overgrowths of cells that develop in the lining of the uterus. They are attached to the uterine wall by a thin stalk or a broader base. These growths can vary in size, ranging from a few millimeters to several centimeters. While most endometrial polyps are non-cancerous, there is a small chance that they could become cancerous, especially in postmenopausal women.
These polyps can occur at any age but are more commonly found in women between the ages of forty and sixty. Some women may have a single polyp, while others may develop multiple growths. The presence of these polyps can interfere with normal menstrual cycles, cause heavy bleeding, or even affect fertility.
Symptoms of Endometrial Polyps
- Irregular menstrual periods
- Heavy or prolonged menstrual bleeding
- Bleeding between periods
- Postmenopausal bleeding
- Difficulty getting pregnant
It is important to note that some women with endometrial polyps may not experience any symptoms at all. In such cases, the polyps are often discovered incidentally during routine gynecological exams or imaging tests.
Potential Causes of Endometrial Polyps
The exact cause of endometrial polyps is not fully understood. However, researchers believe that hormonal imbalances play a significant role in their development. The following factors are thought to contribute to the formation of these growths:
Hormonal Imbalance
Hormones like estrogen and progesterone regulate the growth and shedding of the uterine lining during the menstrual cycle. When there is an imbalance, particularly an excess of estrogen without sufficient progesterone, it can lead to the overgrowth of cells in the endometrium, resulting in polyps.
Inflammation
Chronic inflammation of the uterine lining may also contribute to the development of polyps. Conditions such as endometritis, which is inflammation of the endometrium, can increase the risk of polyp formation.
Age and Menopause
Older women, especially those who are approaching or have gone through menopause, are at a higher risk of developing endometrial polyps. This may be due to changes in hormone levels that occur during this stage of life.
Obesity
Excess body weight is associated with higher levels of estrogen, which can increase the likelihood of developing polyps. Women who are obese may face a greater risk compared to those with a healthy body weight.
Medications
Certain medications, particularly those used for hormone replacement therapy or breast cancer treatment, may elevate the risk of developing endometrial polyps. Tamoxifen, a drug commonly used to treat breast cancer, has been linked to an increased incidence of these growths.
Diagnosing Endometrial Polyps
Diagnosing endometrial polyps typically involves a combination of physical exams, imaging tests, and sometimes surgical procedures. Early and accurate diagnosis is crucial for determining the appropriate treatment plan.
Physical Examination
A healthcare provider may perform a pelvic exam to check for abnormalities in the uterus. While polyps cannot always be felt during a pelvic exam, the doctor may notice signs such as an enlarged or irregularly shaped uterus.
Transvaginal Ultrasound
This imaging test uses sound waves to create detailed pictures of the uterus and its lining. A transvaginal ultrasound can help identify the presence of polyps and provide information about their size and location.
Hysteroscopy
Hysteroscopy is a minimally invasive procedure that allows the doctor to examine the inside of the uterus using a thin, lighted instrument called a hysteroscope. This procedure is often performed in an outpatient setting and provides a direct view of any polyps or other abnormalities.
Endometrial Biopsy
In some cases, a small sample of tissue from the uterine lining may be removed for further analysis. This biopsy can help rule out cancer or other conditions that may mimic the symptoms of endometrial polyps.
Treatment Options for Endometrial Polyps
The treatment approach for endometrial polyps depends on various factors, including the size and number of polyps, the presence of symptoms, and the patient’s age and reproductive goals. Below are some common treatment options:
Watchful Waiting
For women who do not experience symptoms and are not at high risk for complications, a “watch and wait” approach may be recommended. Regular monitoring through follow-up appointments and imaging tests can help ensure that the polyps do not grow or cause problems.
Medications
Hormonal medications, such as progestins, may be prescribed to regulate hormone levels and reduce the size of the polyps. Birth control pills or intrauterine devices that release progestin can also be effective in managing symptoms and preventing recurrence.
Hysteroscopic Polypectomy
This is a minimally invasive surgical procedure used to remove polyps. During the procedure, a hysteroscope is inserted into the uterus, and specialized tools are used to excise the polyps. Hysteroscopic polypectomy is often performed under general anesthesia and is considered safe and effective.
Dilation and Curettage (D&C)
In some cases, a dilation and curettage procedure may be necessary to remove larger polyps or when hysteroscopy is not feasible. During a D&C, the cervix is dilated, and the uterine lining is gently scraped to remove abnormal tissue.
Hysterectomy
A hysterectomy, which involves the surgical removal of the uterus, is typically reserved for severe cases or when cancer is suspected. This option is usually considered only for women who no longer wish to have children and have not responded to other treatments.
Preventing Recurrence of Endometrial Polyps
While it may not always be possible to prevent the formation of endometrial polyps, certain lifestyle changes and medical interventions can help reduce the risk of recurrence:
- Maintaining a healthy weight through diet and exercise
- Managing chronic conditions such as diabetes or hypertension
- Discussing medication options with a healthcare provider to minimize hormonal imbalances
- Regular gynecological check-ups to monitor uterine health
Women who have undergone treatment for endometrial polyps should remain vigilant about any new symptoms and report them promptly to their healthcare provider.
Impact on Fertility
Endometrial polyps can interfere with fertility by disrupting the implantation of a fertilized egg in the uterine lining. In women trying to conceive, the presence of polyps may reduce the chances of successful pregnancy. Removing the polyps through procedures like hysteroscopic polypectomy can improve fertility outcomes and increase the likelihood of conception.
When to Seek Medical Attention
Women experiencing symptoms such as abnormal vaginal bleeding, pelvic pain, or difficulty getting pregnant should consult a healthcare provider. Postmenopausal women who notice any vaginal bleeding should seek immediate medical attention, as this could indicate a more serious underlying condition.
Early diagnosis and treatment of endometrial polyps can help alleviate symptoms, prevent complications, and improve overall quality of life. By staying informed and proactive about reproductive health, women can take important steps toward managing this condition effectively.