Endometrial cancer, often abbreviated as EC, is a type of cancer that begins in the lining of the uterus, known as the endometrium. It is one of the most common gynecological cancers and primarily affects women who have reached menopause. While it is more prevalent in older women, younger women can also be at risk depending on various factors. This article will explore the causes, symptoms, diagnosis, and treatment options for this condition.
What is Endometrial Cancer?
Endometrial cancer starts in the innermost layer of the uterus, which is responsible for thickening during the menstrual cycle to prepare for potential pregnancy. When pregnancy does not occur, the lining sheds during menstruation. In some cases, abnormal cells can develop in this lining, leading to cancerous growths. These growths, if left untreated, can spread to other parts of the body.
Types of Endometrial Cancer
- Type 1: This is the most common form and is often linked to excess estrogen exposure. It tends to grow slowly and has a better prognosis.
- Type 2: This type is less common but more aggressive. It is not typically associated with estrogen levels and often occurs in older women.
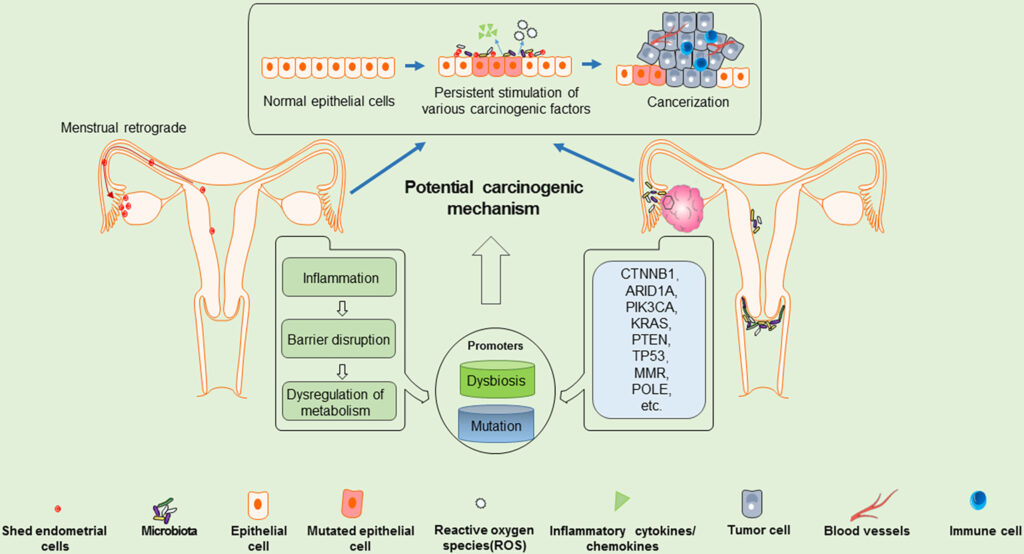
Causes of Endometrial Cancer
The exact cause of endometrial cancer is not fully understood, but several factors are believed to contribute to its development. Understanding these factors can help individuals take preventive measures and seek early medical intervention.
Hormonal Imbalance
A hormonal imbalance, particularly involving estrogen and progesterone, is one of the primary causes of endometrial cancer. Estrogen promotes the growth of the uterine lining, while progesterone helps balance this effect. If there is too much estrogen without enough progesterone, the lining can become too thick, increasing the risk of abnormal cell growth.
Obesity
Obesity is another significant risk factor for endometrial cancer. Fat tissue produces extra estrogen, which can disrupt the hormonal balance in the body. Women who are overweight or obese are at a higher risk of developing this type of cancer compared to those with a healthy weight.
Age
Endometrial cancer is most commonly diagnosed in women over the age of fifty. As women age, their risk increases, especially after menopause when the body experiences changes in hormone levels.
Family History
A family history of endometrial cancer or other related cancers, such as colorectal cancer, can increase an individual’s risk. Some inherited genetic conditions, like Lynch syndrome, are also associated with a higher likelihood of developing this disease.
Other Risk Factors
- Never having been pregnant
- Taking estrogen-only hormone replacement therapy after menopause
- Having polycystic ovary syndrome
- Diabetes
- High blood pressure
Symptoms of Endometrial Cancer
Recognizing the symptoms of endometrial cancer early can lead to timely diagnosis and treatment. The following are some of the most common signs:
Abnormal Vaginal Bleeding
One of the hallmark symptoms of endometrial cancer is abnormal vaginal bleeding. For women who have already gone through menopause, any form of vaginal bleeding should be evaluated by a healthcare provider. In premenopausal women, irregular periods or unusually heavy bleeding may indicate a problem.
Pelvic Pain
Some women with endometrial cancer experience pelvic pain or discomfort. This symptom may not appear until the cancer has progressed, so it is important to report any persistent pain to a doctor.
Pain During Intercourse
Painful intercourse can also be a sign of endometrial cancer. While this symptom can result from other conditions, it should not be ignored, especially if accompanied by other warning signs.
Unexplained Weight Loss
In advanced stages, unexplained weight loss may occur. This symptom is often associated with more aggressive forms of cancer and requires immediate medical attention.
Diagnosis of Endometrial Cancer
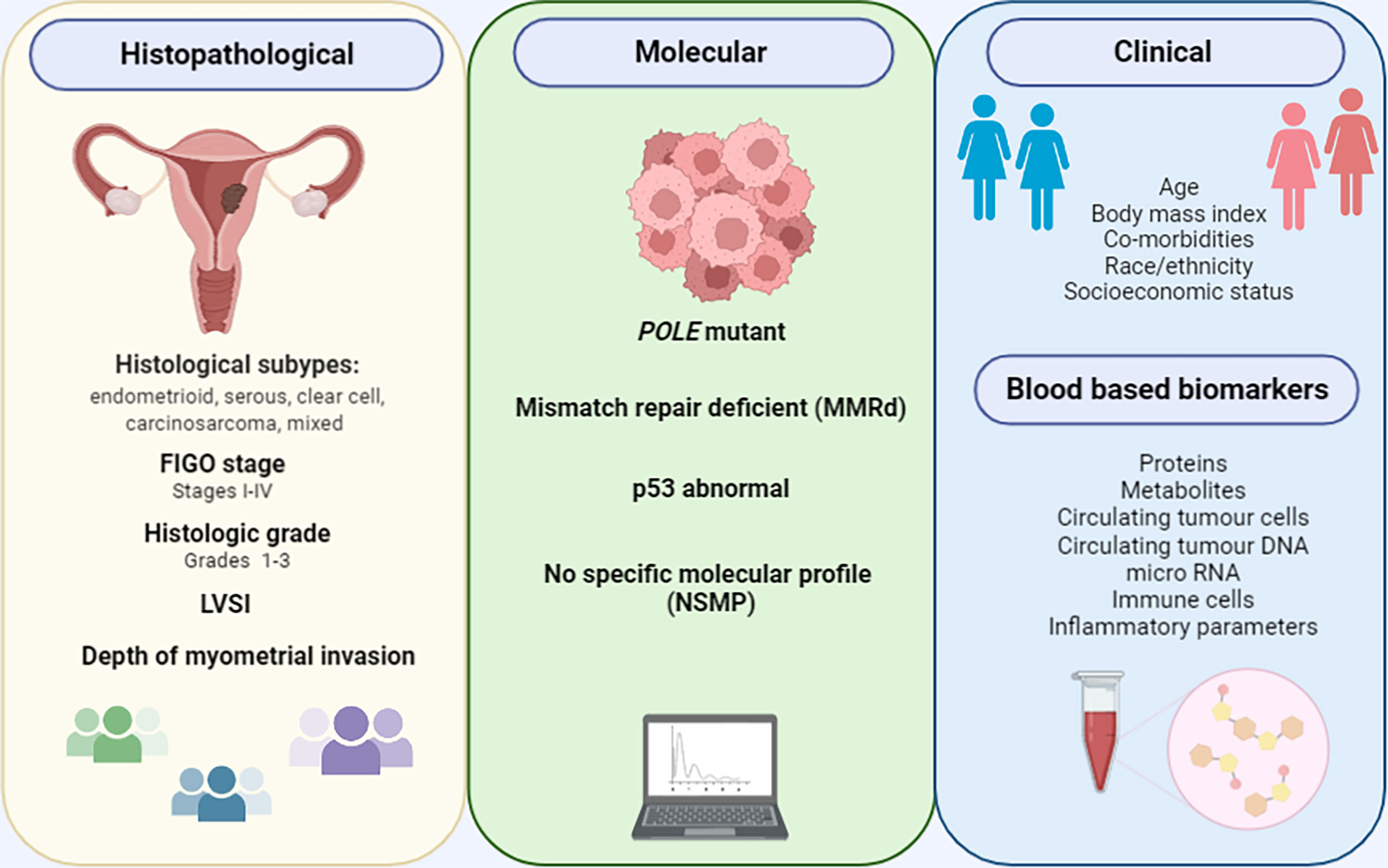
Diagnosing endometrial cancer involves a series of tests and procedures designed to confirm the presence of cancerous cells and determine the extent of the disease. Early diagnosis improves the chances of successful treatment.
Medical History and Physical Examination
The first step in diagnosing endometrial cancer is a thorough review of the patient’s medical history and a physical examination. The doctor will ask about symptoms, risk factors, and family history. A pelvic exam may also be performed to check for abnormalities in the uterus or surrounding areas.
Transvaginal Ultrasound
A transvaginal ultrasound uses sound waves to create images of the uterus and its lining. This test can help identify thickening of the endometrium, which may suggest the presence of cancerous or precancerous cells.
Endometrial Biopsy
An endometrial biopsy involves removing a small sample of tissue from the lining of the uterus. This sample is then examined under a microscope to look for abnormal cells. A biopsy is one of the most reliable ways to diagnose endometrial cancer.
Dilation and Curettage
If the biopsy results are inconclusive, a procedure called dilation and curettage may be performed. During this procedure, the cervix is dilated, and a tool called a curette is used to scrape tissue from the uterine lining for further analysis.
Imaging Tests
Imaging tests, such as magnetic resonance imaging or computed tomography scans, may be used to determine whether the cancer has spread beyond the uterus. These tests provide detailed images of the internal organs and tissues.
Treatment Options for Endometrial Cancer
Treatment for endometrial cancer depends on several factors, including the stage of the disease, the patient’s overall health, and personal preferences. The goal of treatment is to remove or destroy cancerous cells and prevent the cancer from spreading.
Surgery
Surgery is the most common treatment for endometrial cancer. The primary surgical procedure is a hysterectomy, which involves removing the uterus. In many cases, the fallopian tubes and ovaries are also removed. Lymph nodes in the pelvic area may be examined or removed to check for cancer spread.
Radiation Therapy
Radiation therapy uses high-energy beams to kill cancer cells. It may be used before surgery to shrink tumors or after surgery to eliminate any remaining cancer cells. Radiation therapy can also be used as the primary treatment for patients who are not candidates for surgery.
Chemotherapy
Chemotherapy involves the use of drugs to kill cancer cells. It is often recommended for advanced stages of endometrial cancer or when the cancer has spread to other parts of the body. Chemotherapy may be used alone or in combination with radiation therapy.
Hormone Therapy
Hormone therapy is sometimes used to treat certain types of endometrial cancer, particularly those that are sensitive to hormones. This treatment involves medications that block the effects of estrogen or reduce its production in the body.
Targeted Therapy
Targeted therapy focuses on specific weaknesses within cancer cells. By targeting these vulnerabilities, the treatment can stop the cancer cells from growing and spreading. Targeted therapy is often used in combination with other treatments.
Immunotherapy
Immunotherapy works by boosting the body’s immune system to fight cancer. While it is not commonly used for endometrial cancer, it may be an option for certain patients, especially those with advanced or recurrent disease.
Lifestyle Changes and Supportive Care
In addition to medical treatments, making lifestyle changes and seeking supportive care can improve outcomes and quality of life for individuals with endometrial cancer.
Nutrition and Exercise
Maintaining a healthy diet and engaging in regular physical activity can help manage symptoms and improve overall well-being. A balanced diet rich in fruits, vegetables, and whole grains supports the immune system, while exercise can reduce fatigue and stress.
Mental Health Support
Dealing with a cancer diagnosis can be emotionally challenging. Counseling, support groups, and mindfulness practices like meditation can provide emotional relief and help patients cope with the psychological impact of the disease.
Follow-Up Care
Regular follow-up appointments are essential to monitor recovery and detect any recurrence of cancer. These appointments typically include physical exams, imaging tests, and discussions about ongoing symptoms or concerns.