Ehlers-Danlos Syndrome, often abbreviated as EDS, is a group of inherited disorders that primarily affect the connective tissues in the body. These tissues provide support and structure to various parts of the body, including the skin, joints, blood vessels, and organs. While the condition is relatively rare, its impact on those who live with it can be profound. This guide will explore the symptoms, types, and management strategies associated with this complex syndrome.
Understanding Connective Tissue Disorders
Connective tissues are made up of proteins such as collagen, which give strength and elasticity to structures throughout the body. In individuals with Ehlers-Danlos Syndrome, there are defects in the production or structure of these proteins, leading to weakened connective tissues. This can result in a wide range of symptoms, from joint hypermobility to fragile skin and vascular complications.
What Causes Ehlers-Danlos Syndrome?
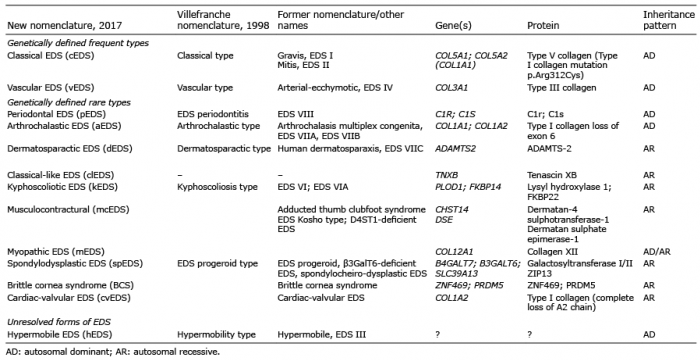
The underlying cause of this condition lies in genetic mutations. These mutations can be inherited from one or both parents or occur spontaneously. The specific gene affected determines the type of syndrome an individual has. Understanding the genetic basis of the disorder is crucial for diagnosis and treatment planning.
Recognizing the Symptoms
The symptoms of this syndrome vary widely depending on the type and severity of the condition. However, some common signs and symptoms are shared across most forms of the disorder. Recognizing these symptoms early can help individuals seek appropriate medical care and improve their quality of life.
Joint Hypermobility
One of the hallmark features of this syndrome is joint hypermobility. People with this condition often have joints that move beyond the normal range of motion. While this may seem like an advantage, it frequently leads to joint instability, frequent dislocations, and chronic pain.
Skin Characteristics
- Stretchy Skin: The skin may appear unusually stretchy and soft to the touch.
- Fragile Skin: It may tear or bruise easily, even with minor trauma.
- Poor Wound Healing: Cuts and injuries may take longer to heal and often leave widened scars.
Vascular Complications
In some types of the syndrome, blood vessels and internal organs can be affected. This can lead to serious complications, such as arterial ruptures, organ perforation, or uterine rupture during pregnancy. These symptoms require immediate medical attention.
Exploring the Different Types
This syndrome is not a single disorder but rather a collection of thirteen distinct types. Each type has unique characteristics and requires tailored management strategies. Below, we explore some of the most common types.
Classical Type
The classical type is characterized by highly elastic, velvety skin that bruises easily. Joint hypermobility is also a prominent feature. Individuals with this type may experience frequent joint dislocations and chronic pain.
Hypermobility Type
The hypermobility type is the most common form of the syndrome. It primarily affects the joints, causing widespread pain, fatigue, and recurrent injuries. Unlike other types, skin involvement is less pronounced in this form.
Vascular Type
The vascular type is considered the most severe form due to its potential to cause life-threatening complications. It affects the walls of blood vessels and internal organs, making them prone to rupture. Early diagnosis and careful monitoring are critical for managing this type.
Kyphoscoliotic Type
This type is marked by severe curvature of the spine (scoliosis) and muscle weakness. Individuals may also experience joint laxity and fragile skin. Respiratory issues can arise due to the spinal deformities.
Dermatosparaxis Type
The dermatosparaxis type is extremely rare and characterized by severely fragile skin that sags and tears easily. Joint hypermobility is less common in this type compared to others.
Diagnosing the Condition
Diagnosing this syndrome can be challenging due to its varied presentation and overlap with other conditions. A thorough evaluation by a healthcare professional is essential. Diagnosis typically involves:
Clinical Evaluation
A doctor will assess symptoms, family history, and physical findings. They may use specific criteria, such as the Beighton score, to evaluate joint hypermobility.
Genetic Testing
Genetic testing can confirm the presence of mutations associated with the syndrome. This is particularly useful for identifying the specific type and guiding treatment decisions.
Imaging Studies
In cases where vascular complications are suspected, imaging studies like ultrasounds or MRIs may be used to assess the condition of blood vessels and internal organs.
Managing the Condition
While there is no cure for this syndrome, effective management strategies can significantly improve quality of life. Treatment plans are tailored to address the specific symptoms and challenges faced by each individual.
Physical Therapy
Physical therapy plays a vital role in managing joint hypermobility and preventing injuries. Strengthening exercises, posture training, and techniques to stabilize joints can reduce pain and improve function.
Pain Management
Chronic pain is a common issue for individuals with this condition. Pain management strategies may include medications, acupuncture, cognitive-behavioral therapy, and lifestyle modifications.
Surgical Interventions
In cases of severe joint instability or vascular complications, surgery may be necessary. However, surgical outcomes can be unpredictable due to the fragility of connective tissues.
Lifestyle Modifications
Making certain lifestyle changes can help manage symptoms effectively:
- Avoid High-Impact Activities: Engage in low-impact exercises like swimming or yoga to protect joints.
- Maintain a Healthy Weight: Excess weight can place additional stress on already vulnerable joints.
- Protect Skin: Use sunscreen, avoid harsh chemicals, and handle skin gently to prevent damage.
Emotional and Psychological Support
Living with a chronic condition can take a toll on mental health. Counseling, support groups, and mindfulness practices can help individuals cope with the emotional challenges of the syndrome.
Raising Awareness and Advocacy
Despite its impact on those affected, this syndrome remains underdiagnosed and misunderstood. Raising awareness about the condition is crucial for improving diagnosis rates and access to care. Advocacy efforts focus on educating healthcare professionals, funding research, and supporting affected individuals and their families.
How You Can Help
- Educate Yourself: Learn more about the condition and share information with others.
- Support Research: Donate to organizations dedicated to studying the syndrome and developing treatments.
- Join a Community: Connect with advocacy groups to find support and contribute to raising awareness.
By understanding the complexities of this syndrome and supporting those who live with it, we can work toward a future where individuals receive timely diagnoses and effective care.