Duchenne Muscular Dystrophy, commonly abbreviated as DMD, is a rare genetic disorder that primarily affects males. It leads to progressive muscle degeneration and weakness, significantly impacting the quality of life for those diagnosed. Understanding the causes, symptoms, progression, and care options for this condition is essential for patients, families, and healthcare providers. In this article, we will delve into these aspects in detail.
What Causes Duchenne Muscular Dystrophy?
The root cause of this condition lies in a mutation in the gene responsible for producing dystrophin, a protein critical for maintaining the integrity of muscle fibers. This gene is located on the X chromosome, which explains why the disorder predominantly affects males. Females have two X chromosomes, so if one carries the mutation, the other typically compensates. Males, however, have only one X chromosome, making them more vulnerable to the effects of the mutation.
The absence or severe deficiency of dystrophin results in the muscles becoming fragile and prone to damage. Over time, the body struggles to repair this damage, leading to muscle wasting and weakness. The genetic mutation responsible for this condition is usually inherited, but in some cases, it can occur spontaneously during conception.
Inheritance Patterns
- X-Linked Recessive Inheritance: Since the gene mutation is located on the X chromosome, mothers who carry the mutation have a fifty percent chance of passing it to their sons, who may develop the disorder. Daughters have a fifty percent chance of becoming carriers.
- Spontaneous Mutations: In approximately one-third of cases, the mutation occurs randomly without any family history of the condition.
Symptoms of Duchenne Muscular Dystrophy
The symptoms of this condition typically begin to appear in early childhood, often between the ages of two and five. These symptoms progress over time and can vary in severity from person to person. Early recognition of these signs is crucial for timely intervention and management.
Early Signs
- Delayed Motor Milestones: Children with this condition may take longer than usual to sit, stand, or walk. They might also struggle with climbing stairs or running.
- Frequent Falls: Due to muscle weakness, children may fall more often than their peers.
- Gower’s Sign: A distinctive way of rising from the floor where the child uses their hands and arms to “walk” up their legs due to weak hip and thigh muscles.
Progressive Symptoms
- Muscle Weakness: As the disease advances, muscle weakness becomes more pronounced, affecting the ability to perform daily activities.
- Difficulty Walking: Many children lose the ability to walk independently by their early teens.
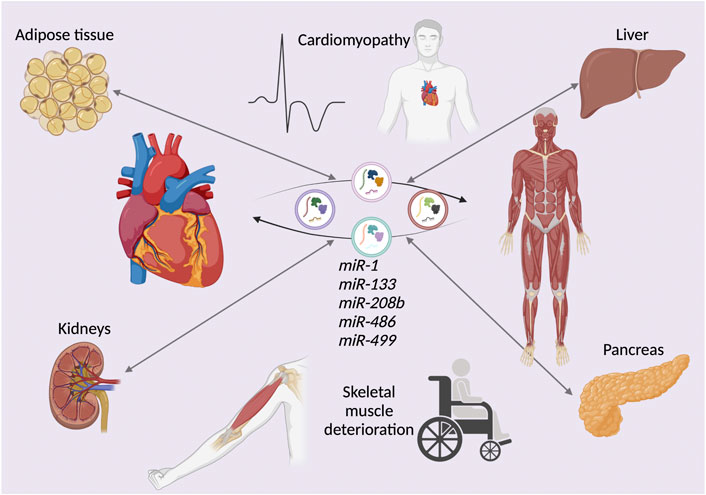
- Cardiac and Respiratory Issues: The heart and respiratory muscles are also affected, leading to complications such as cardiomyopathy and breathing difficulties.
Progression of the Condition
This condition follows a predictable pattern of progression, although the rate at which it advances can differ among individuals. Understanding this progression helps caregivers and healthcare providers plan appropriate interventions and support.
Childhood Stage
In the early years, muscle weakness primarily affects the lower limbs. Children may experience difficulty with activities that require strength and coordination, such as jumping or climbing. Despite these challenges, many children remain ambulatory during this stage.
Adolescent Stage
As the condition progresses into adolescence, muscle weakness spreads to the upper body. Most individuals lose the ability to walk independently and require the use of wheelchairs. During this stage, cardiac and respiratory complications become more apparent and require careful monitoring.
Adult Stage
In adulthood, the focus shifts to managing complications such as heart failure, respiratory insufficiency, and skeletal deformities. While advancements in medical care have improved life expectancy, individuals with this condition still face significant health challenges that necessitate ongoing support.
Care Options for Managing Duchenne Muscular Dystrophy
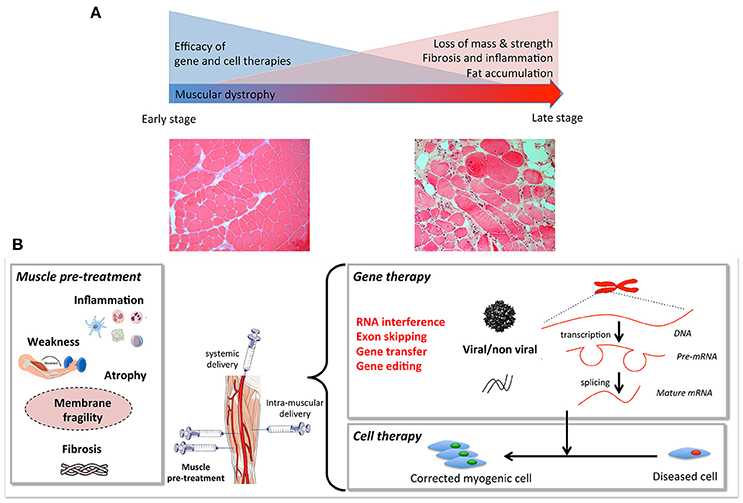
While there is currently no cure for this condition, a multidisciplinary approach to care can help manage symptoms, slow progression, and improve quality of life. Treatment plans are tailored to the individual’s needs and may involve a combination of therapies, medications, and supportive care.
Medical Treatments
- Corticosteroids: Medications such as prednisone and deflazacort are commonly prescribed to slow muscle degeneration and improve strength. However, long-term use may have side effects, including weight gain and bone fragility.
- Gene Therapies: Emerging treatments aim to address the underlying genetic mutation. For example, exon-skipping therapies target specific mutations to restore partial dystrophin production.
Physical and Occupational Therapy
Therapies play a vital role in maintaining mobility and independence for as long as possible. Physical therapy focuses on strengthening muscles and preventing joint contractures, while occupational therapy helps individuals adapt to daily living challenges.
- Stretching Exercises: Regular stretching can prevent stiffness and maintain flexibility.
- Assistive Devices: Wheelchairs, braces, and other aids can enhance mobility and independence.
Cardiac and Respiratory Care
Monitoring and managing heart and lung function are critical components of care. Regular check-ups with cardiologists and pulmonologists help detect and address complications early.
- Medications for Heart Health: Drugs such as ACE inhibitors and beta-blockers may be prescribed to manage cardiomyopathy.
- Respiratory Support: Non-invasive ventilation devices can assist with breathing difficulties, especially during sleep.
Nutritional Support
A balanced diet is essential for overall health and managing symptoms. Nutritional counseling can help address issues such as weight management and swallowing difficulties.
- High-Calorie Diets: For individuals with difficulty maintaining weight, calorie-dense foods may be recommended.
- Swallowing Therapy: Speech therapists can provide strategies to manage swallowing challenges and reduce the risk of aspiration.
Psychological and Emotional Support
Living with this condition can be emotionally challenging for both patients and their families. Counseling and support groups offer valuable resources for coping with the psychological impact of the disorder.
- Individual Counseling: Therapy sessions can help individuals process emotions and develop coping strategies.
- Family Support Groups: Connecting with others facing similar challenges fosters a sense of community and shared understanding.
Educational and Social Support
Ensuring access to education and social opportunities is crucial for fostering independence and self-esteem. Schools and communities can play a key role in creating inclusive environments.
- Individualized Education Plans: Tailored learning plans accommodate physical limitations and learning needs.
- Accessible Facilities: Modifications such as ramps and elevators enable participation in school and community activities.
Ongoing Research and Future Directions
Research into this condition is ongoing, with scientists exploring innovative approaches to treatment and management. Advances in gene editing technologies, such as CRISPR, hold promise for addressing the root cause of the disorder. Clinical trials are also evaluating new therapies aimed at improving muscle function and slowing disease progression.
Collaboration between researchers, healthcare providers, and advocacy organizations continues to drive progress in understanding and treating this condition. Increased awareness and funding are essential to accelerate these efforts and improve outcomes for affected individuals.