Deep Vein Thrombosis, commonly abbreviated as DVT, is a serious medical condition that occurs when a blood clot forms in one or more of the deep veins in the body, typically in the legs. This condition can lead to life-threatening complications if not addressed promptly. Understanding its causes, recognizing its symptoms, and being aware of the available diagnostic methods and treatments are crucial for managing this condition effectively.
What is Deep Vein Thrombosis?
Deep vein thrombosis refers to the formation of a blood clot in the deep veins, most commonly in the legs. These clots can partially or completely block blood flow, leading to pain, swelling, and other complications. If a piece of the clot breaks loose and travels through the bloodstream to the lungs, it can cause a pulmonary embolism, which is a potentially fatal condition.
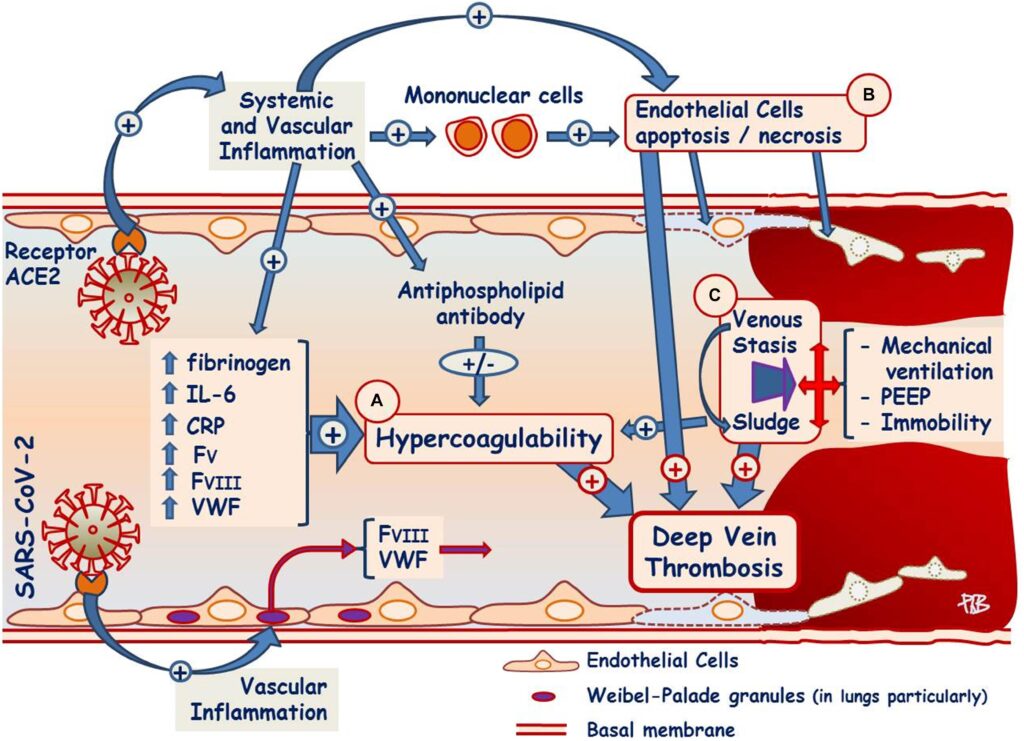
Why Does Deep Vein Thrombosis Occur?
The primary reason behind the development of this condition lies in the disruption of normal blood flow. Blood clots form when certain factors interfere with the body’s natural ability to regulate clotting. There are three main elements that contribute to the formation of these clots:
- Blood Flow Stagnation: When blood flow slows down, it increases the likelihood of clot formation. This often happens during prolonged periods of inactivity, such as long flights, bed rest after surgery, or sitting for extended periods.
- Vessel Wall Damage: Any injury to the inner lining of a vein can trigger clot formation. This damage can result from surgery, trauma, or certain medical conditions.
- Hyperviscosity of Blood: Some individuals have blood that is thicker than normal, making it more prone to clotting. This can be due to genetic predispositions, certain medications, or underlying health conditions.
Common Causes of Deep Vein Thrombosis
There are several factors that increase the risk of developing this condition. While some causes are related to lifestyle choices, others may be linked to medical conditions or external circumstances. Below are some of the most common causes:
Prolonged Immobility
One of the leading causes of clot formation is prolonged immobility. When you sit or lie down for extended periods without moving, blood flow in the legs can slow down significantly. This stagnation creates an environment where clots are more likely to form. Examples include:
- Long-distance travel, especially on airplanes or cars
- Extended bed rest after surgery or illness
- Paralysis or limited mobility due to neurological conditions
Surgical Procedures
Certain types of surgeries, particularly those involving the hips, knees, or abdomen, can increase the risk of clot formation. During surgery, the body’s natural clotting mechanisms are activated to prevent excessive bleeding. However, this can sometimes lead to the unintended formation of clots in the deep veins.
Medical Conditions
Several medical conditions are known to elevate the risk of developing this condition. These include:
- Cancer: Certain types of cancer and their treatments can increase the likelihood of clot formation.
- Heart Failure: Reduced heart function can lead to poor circulation, increasing the risk of clots.
- Inflammatory Bowel Disease: Conditions like Crohn’s disease and ulcerative colitis can affect blood clotting mechanisms.
- Obesity: Excess weight puts additional pressure on the veins in the legs, impairing blood flow.
Hormonal Factors
Hormonal changes can also play a role in the development of this condition. For example:
- Pregnancy increases the pressure on the veins in the pelvis and legs, raising the risk of clot formation.
- The use of birth control pills or hormone replacement therapy can alter the body’s clotting mechanisms.
Symptoms of Deep Vein Thrombosis
Not everyone with this condition experiences noticeable symptoms. In fact, some individuals may have no signs at all, making the condition difficult to detect. However, when symptoms do occur, they often include:
Swelling
One of the most common symptoms is swelling in the affected leg. This swelling usually occurs in one leg rather than both and can range from mild to severe.
Pain
Pain is another frequent symptom. It often starts in the calf and may feel like cramping or soreness. The pain may worsen when standing or walking.
Redness and Warmth
The skin over the affected area may appear red or discolored. Additionally, the area might feel warm to the touch compared to the surrounding skin.
Other Symptoms
In some cases, individuals may experience:
- A feeling of heaviness in the affected leg
- Visible surface veins
- Fatigue or discomfort in the leg
Diagnosis of Deep Vein Thrombosis
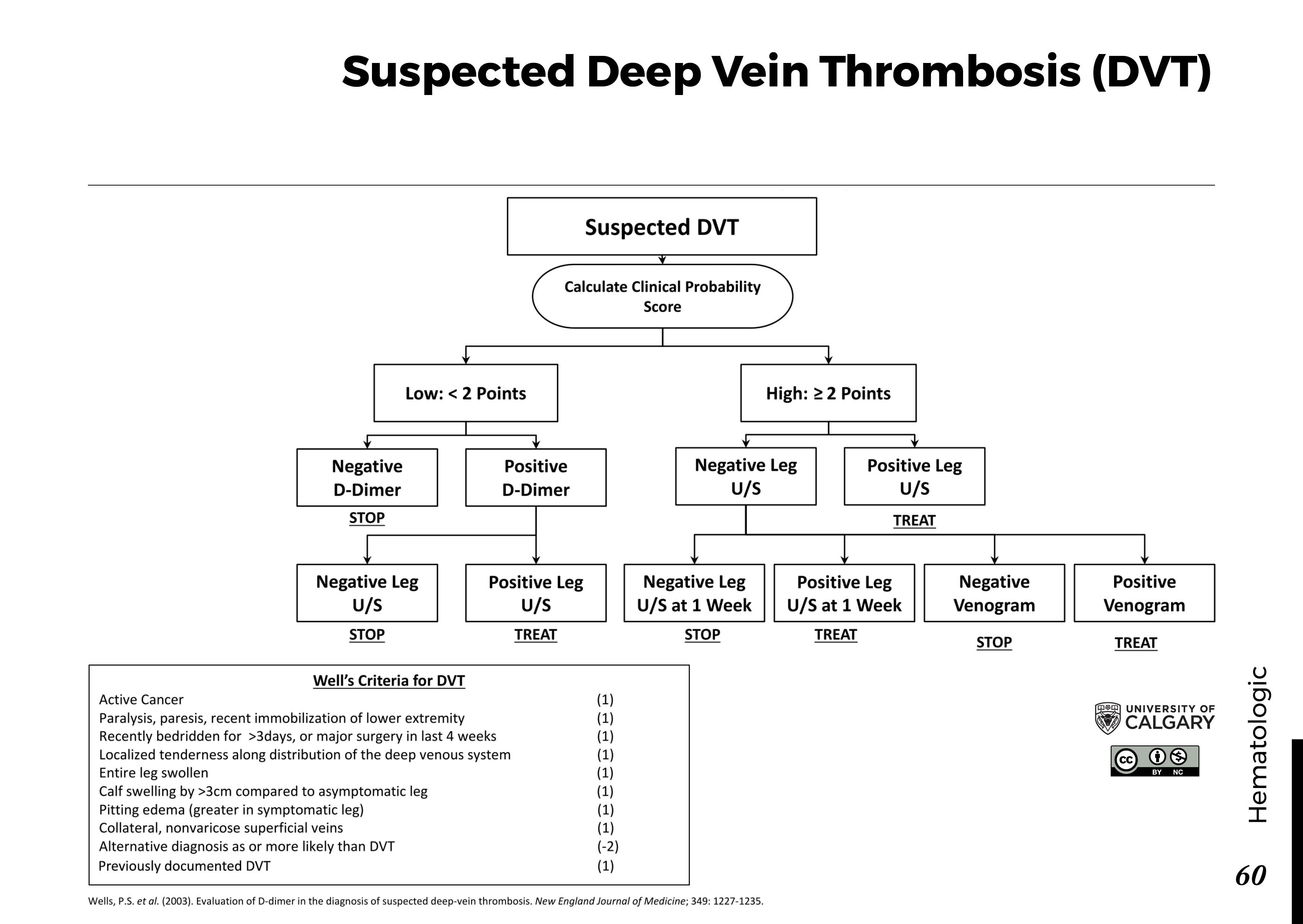
Early diagnosis is critical to prevent complications. If a healthcare provider suspects this condition, they will typically perform a series of tests to confirm the presence of a clot. These diagnostic methods include:
Physical Examination
A physical examination is often the first step. The healthcare provider will check for signs of swelling, tenderness, or discoloration in the legs. They may also ask about any recent activities or medical history that could indicate a higher risk.
Ultrasound
An ultrasound is one of the most common diagnostic tools used to detect this condition. This non-invasive test uses sound waves to create images of the veins and identify any blockages caused by clots.
Blood Tests
Blood tests can help determine whether the body is producing elevated levels of certain substances associated with clot formation. One such test measures D-dimer levels, a protein fragment that is released when a clot dissolves.
Venography
In some cases, a venography may be performed. This involves injecting a dye into the veins and taking X-rays to visualize blood flow and identify any obstructions.
Magnetic Resonance Imaging (MRI)
An MRI may be used in complex cases or when the clot is located in areas that are difficult to assess with other methods. This imaging technique provides detailed pictures of the veins and surrounding tissues.
Treatment Options for Deep Vein Thrombosis
Once diagnosed, prompt treatment is essential to prevent complications such as pulmonary embolism. The primary goals of treatment are to stop the clot from growing, prevent new clots from forming, and reduce the risk of complications. Common treatment options include:
Anticoagulant Medications
Anticoagulants, also known as blood thinners, are the most common treatment for this condition. These medications work by reducing the blood’s ability to clot, thereby preventing existing clots from growing larger and stopping new ones from forming. Examples include:
- Heparin: Often administered intravenously in a hospital setting.
- Warfarin: Taken orally and requires regular monitoring of blood levels.
- Newer oral anticoagulants: Such as rivaroxaban and apixaban, which do not require frequent monitoring.
Compression Stockings
Compression stockings are tight-fitting garments that apply gentle pressure to the legs. They help improve blood flow and reduce the risk of swelling and complications. These stockings are typically worn during the day and removed at night.
Thrombolytic Therapy
In severe cases where the clot is large or causing significant symptoms, thrombolytic therapy may be used. This treatment involves administering medications that dissolve the clot quickly. However, it carries a higher risk of bleeding and is usually reserved for life-threatening situations.
Inferior Vena Cava Filter
For individuals who cannot take blood thinners or who continue to develop clots despite treatment, an inferior vena cava filter may be inserted. This device is placed in the largest vein in the body to catch any clots before they reach the lungs.
Lifestyle Changes
In addition to medical treatments, making certain lifestyle changes can help manage this condition and reduce the risk of recurrence. These include:
- Regular exercise to improve circulation
- Maintaining a healthy weight
- Avoiding prolonged periods of inactivity
- Staying hydrated, especially during long trips
Surgical Intervention
In rare cases, surgery may be required to remove a clot. This procedure, known as thrombectomy, is typically performed in emergency situations where the clot poses an immediate threat to life.
Preventing Deep Vein Thrombosis
While not all cases of this condition can be prevented, there are steps individuals can take to lower their risk. These preventive measures are particularly important for those with known risk factors:
- Move around regularly, especially during long trips or periods of inactivity.
- Exercise the legs while sitting by flexing and extending the ankles.
- Wear compression stockings if recommended by a healthcare provider.
- Follow a healthy diet and maintain a healthy weight.
- Discuss any family history of clotting disorders with your doctor.