Congenital Heart Defects, commonly abbreviated as CHD, refer to structural abnormalities in the heart that are present at birth. These defects can range from mild conditions that may not require treatment to severe ones that necessitate immediate medical intervention. Understanding the different types, causes, symptoms, and available treatments for these defects is crucial for early diagnosis and effective management. In this article, we will delve into the intricacies of congenital heart defects to provide a comprehensive overview.
Understanding Congenital Heart Defects
Congenital heart defects occur when the heart or the blood vessels near the heart do not develop properly before birth. These defects can affect the walls of the heart, the valves, or the arteries and veins near the heart. While some defects are minor and may go unnoticed for years, others can cause life-threatening complications shortly after birth.
How Common Are Congenital Heart Defects?
Congenital heart defects are among the most common types of birth defects. It is estimated that about one percent of all babies are born with some form of heart abnormality. Advances in medical technology have significantly improved survival rates, allowing many individuals with congenital heart defects to live long and healthy lives.
Types of Congenital Heart Defects
There are several types of congenital heart defects, each affecting different parts of the heart. Below are some of the most common types:
Septal Defects
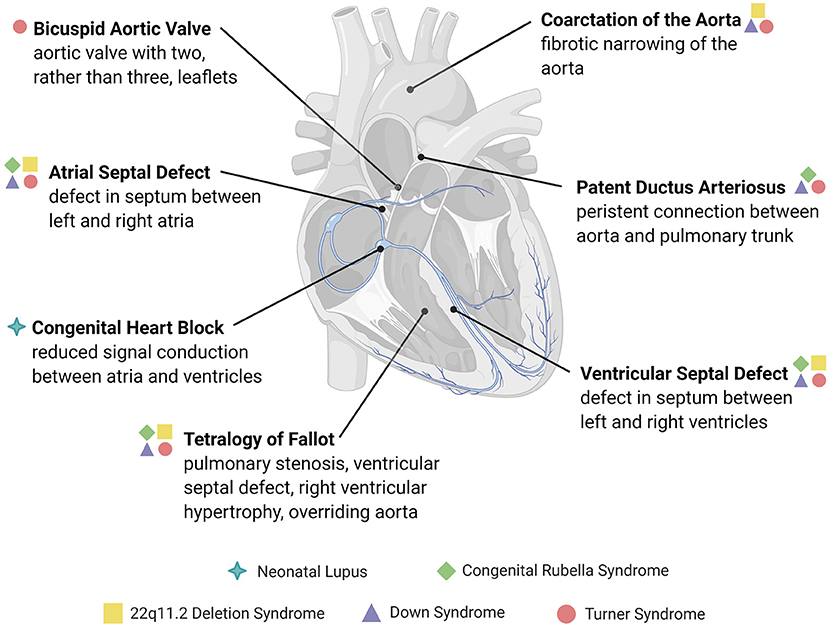
- Ventricular Septal Defect: This occurs when there is a hole in the wall separating the two lower chambers of the heart, known as the ventricles. The hole allows oxygen-rich blood to mix with oxygen-poor blood, which can lead to inefficient circulation.
- Atrial Septal Defect: In this condition, there is a hole in the wall separating the two upper chambers of the heart, called the atria. Similar to ventricular septal defects, this allows blood to mix between the two sides of the heart.
Valve Abnormalities
- Pulmonary Valve Stenosis: This defect involves the narrowing of the pulmonary valve, which controls blood flow from the heart to the lungs. When the valve is too narrow, it forces the heart to work harder to pump blood.
- Aortic Valve Stenosis: This condition affects the aortic valve, which regulates blood flow from the heart to the rest of the body. A narrowed aortic valve can restrict blood flow and strain the heart.
Cyanotic Heart Defects
- Tetralogy of Fallot: This is a combination of four related heart defects, including a ventricular septal defect, pulmonary valve stenosis, an overriding aorta, and thickening of the right ventricle. These defects together cause low oxygen levels in the blood, leading to a bluish tint to the skin, known as cyanosis.
- Transposition of the Great Arteries: In this condition, the two main arteries leaving the heart are reversed. This results in oxygen-poor blood being pumped back into the body instead of going to the lungs for oxygenation.
Other Types
- Coarctation of the Aorta: This defect involves the narrowing of the aorta, the main artery that carries blood from the heart to the body. Narrowing restricts blood flow and increases blood pressure in the upper body.
- Hypoplastic Left Heart Syndrome: In this rare and serious condition, the left side of the heart is severely underdeveloped. As a result, the heart cannot effectively pump blood to the body.
Causes of Congenital Heart Defects
The exact cause of congenital heart defects is often unknown. However, research has identified several factors that may contribute to their development:
Genetic Factors
In some cases, congenital heart defects are linked to genetic conditions. For example, Down syndrome, Turner syndrome, and other chromosomal abnormalities are associated with an increased risk of heart defects. Additionally, if a parent or sibling has a congenital heart defect, the likelihood of the condition occurring in other family members is higher.
Environmental Factors
Certain environmental factors during pregnancy can increase the risk of congenital heart defects. These include:
- Maternal Infections: Infections such as rubella (German measles) during pregnancy can interfere with fetal heart development.
- Medications: Some medications taken during pregnancy, such as certain acne drugs, anticonvulsants, and lithium, have been linked to an increased risk of heart defects.
- Substance Use: Smoking, alcohol consumption, and drug use during pregnancy can harm fetal development, including the heart.
Maternal Health Conditions
Pre-existing health conditions in the mother can also play a role. For instance, diabetes and phenylketonuria (PKU) that are poorly controlled during pregnancy can increase the risk of congenital heart defects in the baby.
Symptoms of Congenital Heart Defects
The symptoms of congenital heart defects vary depending on the type and severity of the condition. Some defects may not cause noticeable symptoms until later in life, while others are apparent shortly after birth. Common symptoms include:
- Cyanosis, or a bluish tint to the skin, lips, or fingernails
- Rapid breathing or shortness of breath
- Fatigue or difficulty feeding in infants
- Poor weight gain
- Swelling in the legs, abdomen, or around the eyes
- Heart murmurs, which are abnormal sounds heard during a heartbeat
Symptoms in Adults
While many congenital heart defects are diagnosed in infancy, some individuals may not experience symptoms until adulthood. In such cases, symptoms may include:
- Shortness of breath during exercise or physical activity
- Heart palpitations or irregular heartbeats
- Fainting or dizziness
- Swelling in the hands, feet, or ankles
Treatments for Congenital Heart Defects
Treatment options for congenital heart defects depend on the type and severity of the condition. In some cases, mild defects may not require treatment and can be monitored regularly. For more serious defects, medical interventions may be necessary.
Medications
Medications are often used to manage symptoms and improve heart function. Common medications include:
- Diuretics: These help reduce fluid buildup in the body by increasing urine production.
- Beta-Blockers: These slow the heart rate and reduce the workload on the heart.
- Anticoagulants: These prevent blood clots from forming, which is especially important for individuals with artificial heart valves or certain types of defects.
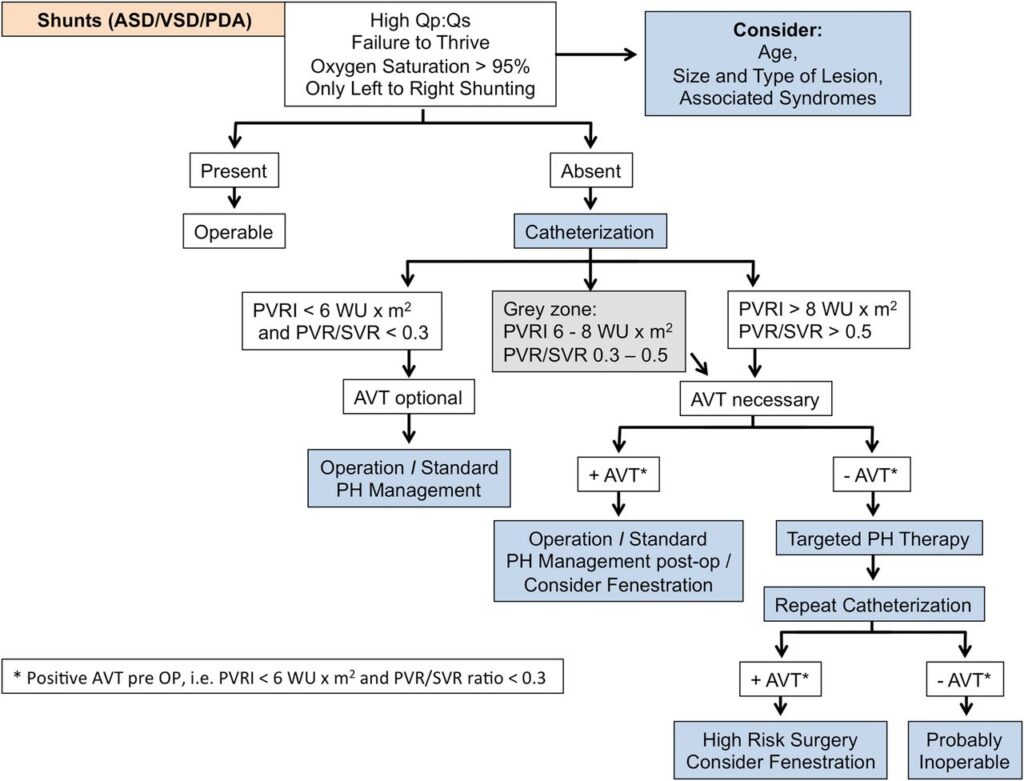
Catheter Procedures
Catheter-based procedures are minimally invasive treatments that involve inserting a thin tube into a blood vessel and guiding it to the heart. These procedures can be used to repair certain types of defects, such as closing holes in the heart or widening narrowed valves or arteries.
Surgical Interventions
In more severe cases, open-heart surgery may be required to repair or replace damaged heart structures. Examples of surgical procedures include:
- Patching Holes in the Heart: Surgeons use patches to close septal defects and restore normal blood flow.
- Valve Repair or Replacement: Damaged valves can be repaired or replaced with artificial or donor valves.
- Correcting Complex Defects: For conditions like hypoplastic left heart syndrome, multiple surgeries may be needed to reroute blood flow and support heart function.
Heart Transplants
In rare and severe cases where the heart is too damaged to be repaired, a heart transplant may be necessary. This involves replacing the defective heart with a healthy donor heart.
Lifestyle Management
In addition to medical treatments, individuals with congenital heart defects may benefit from lifestyle changes to improve their overall health. These include:
- Maintaining a heart-healthy diet low in salt and saturated fats
- Engaging in regular, moderate exercise as recommended by a healthcare provider
- Avoiding smoking and excessive alcohol consumption
- Regular follow-up appointments with a cardiologist to monitor heart health
Advances in Diagnosis and Treatment
Recent advancements in medical technology have greatly improved the diagnosis and treatment of congenital heart defects. Techniques such as echocardiography, magnetic resonance imaging (MRI), and computed tomography (CT) scans allow doctors to visualize the heart’s structure and function in detail. Additionally, innovations in surgical techniques and catheter-based interventions have made treatments safer and more effective.
Research continues to explore new therapies, including stem cell therapy and gene editing, which hold promise for repairing damaged heart tissue and addressing the root causes of congenital heart defects.