Chronic wounds are a significant health concern worldwide, affecting millions of people and posing challenges for both patients and healthcare providers. These wounds, which fail to progress through the normal stages of healing in a timely manner, can lead to severe complications if left untreated. In this article, we will explore the different types of chronic wounds, their underlying causes, and the complex process of wound healing. Understanding these aspects is crucial for effective management and treatment.
Understanding Chronic Wounds
Chronic wounds are defined as wounds that do not heal within the expected timeframe, typically three months or more. Unlike acute wounds, which follow a predictable healing process, chronic wounds often stall in one of the healing stages due to various factors such as underlying health conditions, poor circulation, or infection. This delay can result in prolonged pain, increased risk of infection, and reduced quality of life for affected individuals.
Types of Chronic Wounds
There are several types of chronic wounds, each with unique characteristics and causes. Below are some of the most common types:
Pressure Ulcers
Pressure ulcers, also known as bedsores, occur when prolonged pressure is applied to a specific area of the body, usually over bony prominences like the hips, heels, or tailbone. These wounds are commonly seen in individuals who are bedridden or use wheelchairs for extended periods. The constant pressure reduces blood flow to the affected area, leading to tissue damage and ulceration.
Diabetic Foot Ulcers
Diabetic foot ulcers are a frequent complication of diabetes, particularly in individuals with poorly controlled blood sugar levels. High glucose levels can cause nerve damage, resulting in a loss of sensation in the feet. This lack of sensation makes it difficult for individuals to detect injuries or pressure points, increasing the risk of developing ulcers. Poor circulation further complicates the healing process, making these wounds particularly challenging to treat.
Venous Leg Ulcers
Venous leg ulcers are caused by poor circulation in the veins of the legs. When the veins fail to return blood to the heart effectively, pressure builds up in the lower extremities, leading to swelling and skin breakdown. These ulcers are often accompanied by symptoms such as leg pain, heaviness, and discoloration of the skin. Individuals with a history of deep vein thrombosis or varicose veins are at higher risk of developing venous leg ulcers.
Arterial Ulcers
Arterial ulcers result from insufficient blood flow to the tissues due to blocked or narrowed arteries. These wounds typically occur on the toes, feet, or lower legs and are characterized by a punched-out appearance with well-defined edges. Arterial ulcers are often painful, especially at night, and may be associated with other symptoms such as cold extremities and delayed capillary refill.
Causes of Chronic Wounds
Several factors contribute to the development and persistence of chronic wounds. Understanding these causes is essential for effective prevention and treatment.
Poor Circulation
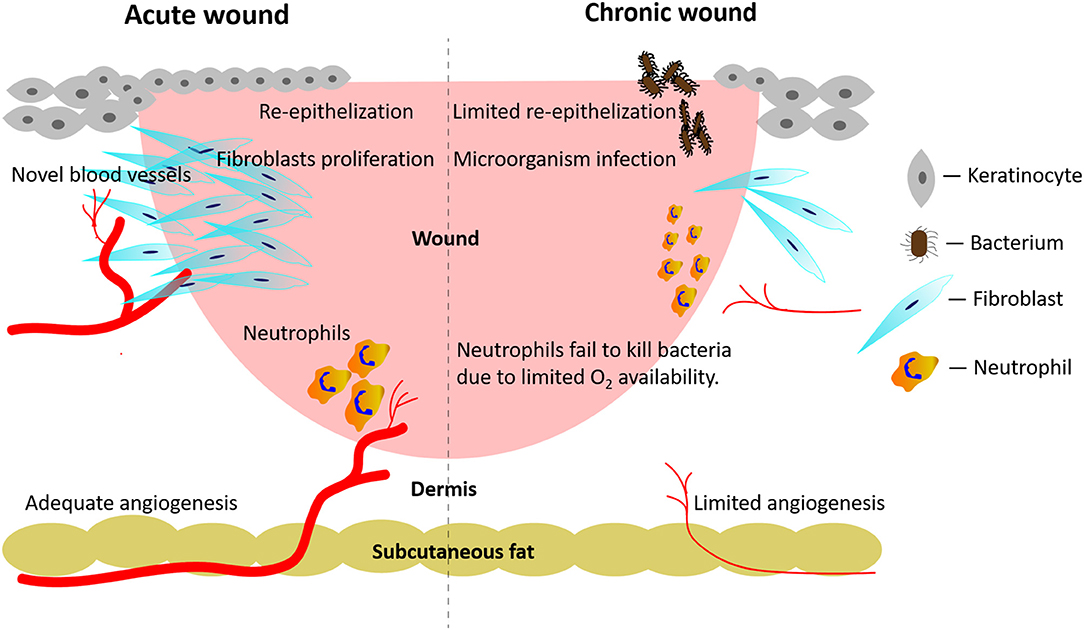
Circulation plays a critical role in wound healing. Blood delivers oxygen and nutrients to the damaged tissues, promoting repair and regeneration. When circulation is impaired, either due to arterial disease or venous insufficiency, the healing process is disrupted. This can lead to the formation of chronic wounds that are slow to heal or prone to recurring.
Infection
Infections are a common complication of chronic wounds. Bacteria can colonize the wound site, causing inflammation and delaying the healing process. If left untreated, infections can spread to surrounding tissues or even enter the bloodstream, leading to life-threatening conditions such as sepsis. Proper wound care and regular monitoring are essential to prevent and manage infections.
Underlying Health Conditions
Several health conditions increase the risk of developing chronic wounds. Diabetes, for example, affects blood sugar levels and nerve function, making individuals more susceptible to foot ulcers. Similarly, autoimmune diseases like rheumatoid arthritis can impair the immune system, reducing the body’s ability to heal wounds effectively. Obesity, smoking, and malnutrition are additional risk factors that can compromise the healing process.
Trauma or Injury
Traumatic injuries, such as burns or deep cuts, can sometimes lead to chronic wounds if they are not treated promptly or if complications arise during the healing process. For instance, improper wound care or the presence of foreign objects in the wound can interfere with healing, resulting in a chronic condition.
The Healing Process of Chronic Wounds
The healing process of chronic wounds is complex and involves several overlapping stages. While acute wounds typically progress through these stages in a linear fashion, chronic wounds often experience delays or disruptions at one or more stages.
Hemostasis
Hemostasis is the first stage of wound healing and occurs immediately after injury. During this phase, the body works to stop bleeding by constricting blood vessels and forming a clot. Platelets play a crucial role in this process by aggregating at the wound site and releasing growth factors that initiate the next stages of healing.
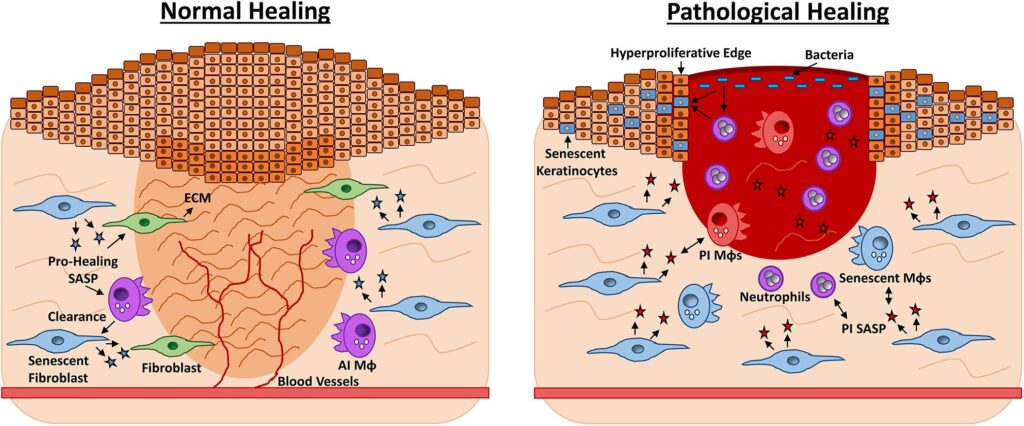
Inflammation
The inflammatory phase follows hemostasis and is characterized by redness, swelling, warmth, and pain at the wound site. During this stage, white blood cells, such as neutrophils and macrophages, migrate to the area to remove debris and fight infection. This phase is essential for preparing the wound bed for the subsequent stages of healing.
Proliferation
Proliferation is the phase where new tissue begins to form. Fibroblasts produce collagen, a structural protein that provides strength and support to the healing tissue. New blood vessels also develop during this stage, a process known as angiogenesis, to restore blood flow to the area. Epithelial cells migrate across the wound surface, gradually closing the gap and forming a protective barrier.
Remodeling
The final stage of wound healing is remodeling, during which the newly formed tissue matures and strengthens. Collagen fibers reorganize to improve the tensile strength of the scar tissue. This phase can last for months or even years, depending on the severity of the wound and the individual’s overall health.
Factors Affecting the Healing Process
Several factors can influence the healing process of chronic wounds, either positively or negatively. Addressing these factors is key to promoting optimal healing outcomes.
Nutrition
Adequate nutrition is essential for wound healing. Proteins, vitamins, and minerals such as zinc and vitamin C play vital roles in collagen synthesis, immune function, and cell regeneration. Malnutrition or deficiencies in these nutrients can significantly impair the healing process, prolonging the duration of chronic wounds.
Oxygenation
Oxygen is critical for energy production and cellular activity during wound healing. Conditions that reduce oxygen delivery to the tissues, such as anemia or respiratory disorders, can hinder the healing process. Hyperbaric oxygen therapy is sometimes used to enhance oxygenation and promote healing in chronic wounds.
Wound Care Practices
Proper wound care is essential for preventing complications and supporting the healing process. This includes regular cleaning and dressing changes, debridement of dead tissue, and the use of advanced wound care products such as hydrogels or antimicrobial dressings. Neglecting these practices can lead to infection, delayed healing, or worsening of the wound.
Psychological Factors
Psychological stress and mental health conditions can also impact wound healing. Chronic stress has been shown to suppress the immune system and increase inflammation, both of which can impede the healing process. Providing emotional support and addressing mental health concerns can improve outcomes for individuals with chronic wounds.