Chronic Obstructive Pulmonary Disease, commonly known as COPD, is a progressive lung condition that affects millions of people worldwide. It encompasses a group of respiratory disorders that make it difficult to breathe and significantly impact the quality of life. This article provides an in-depth look into this condition, exploring its causes, symptoms, and care strategies to help individuals better understand and manage it.
Understanding Chronic Obstructive Pulmonary Disease
Chronic Obstructive Pulmonary Disease refers to a group of lung conditions that cause airflow blockage and breathing-related problems. The two most common forms of this disease are emphysema and chronic bronchitis. Emphysema involves damage to the air sacs in the lungs, while chronic bronchitis is characterized by inflammation and narrowing of the airways. Both conditions often occur together and contribute to the overall progression of the disease.
This condition develops slowly over time and is typically diagnosed in individuals who are middle-aged or older. While it is not curable, proper management can slow its progression and improve daily functioning.
What Happens in the Lungs?
- Airflow becomes restricted due to inflammation and thickening of the airways.
- Damaged air sacs lose their elasticity, making it harder for air to move in and out of the lungs.
- Mucus production increases, further obstructing the airways.
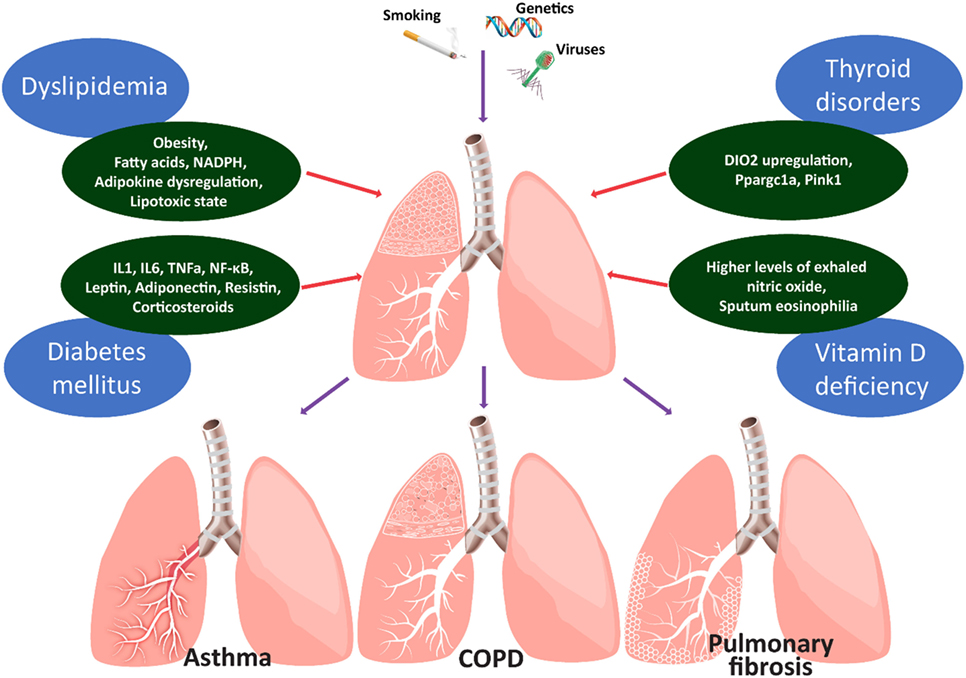
Causes of Chronic Obstructive Pulmonary Disease
The primary cause of this respiratory condition is long-term exposure to irritants that damage the lungs and airways. Understanding these causes is crucial for prevention and early intervention.
Tobacco Smoke
Cigarette smoking is the leading cause of this lung disease. Approximately 85-90% of all cases are linked to smoking. Whether someone smokes cigarettes, cigars, or pipes, the harmful chemicals in tobacco smoke irritate and inflame the airways, leading to permanent damage over time. Secondhand smoke exposure can also increase the risk, even for nonsmokers.
Environmental Factors
Prolonged exposure to air pollution, chemical fumes, dust, and other airborne irritants in the workplace or home environment can contribute to the development of this condition. Occupations such as mining, construction, and manufacturing often expose workers to harmful particles that can damage the lungs.
Genetic Predisposition
In rare cases, a genetic condition called alpha-1 antitrypsin deficiency can lead to the development of this disease. Alpha-1 antitrypsin is a protein that protects the lungs from damage. Individuals with low levels of this protein are more susceptible to lung diseases, even if they have never smoked or been exposed to environmental pollutants.
Other Contributing Factors
- Frequent respiratory infections during childhood.
- Asthma that is poorly managed or untreated.
- Long-term use of cooking fuels that produce indoor air pollution, particularly in developing countries.
Symptoms of Chronic Obstructive Pulmonary Disease
The symptoms of this lung condition often develop gradually and worsen over time. Early recognition of these signs can lead to timely diagnosis and treatment, improving outcomes for affected individuals.
Common Symptoms
- Shortness of breath, especially during physical activities.
- Chronic cough, often referred to as a “smoker’s cough.”
- Excessive mucus production, which may be clear, white, yellow, or greenish.
- Wheezing or a whistling sound when breathing.
- Chest tightness or discomfort.
Advanced Symptoms
As the disease progresses, individuals may experience more severe symptoms, including:
- Frequent respiratory infections.
- Swelling in the ankles, feet, or legs due to fluid retention.
- Unintended weight loss.
- Difficulty performing everyday tasks due to extreme fatigue.
When to Seek Medical Attention
If you or a loved one experiences any of the following, it is important to seek medical attention immediately:
- Sudden worsening of symptoms, such as increased shortness of breath or excessive mucus production.
- Bluish discoloration of the lips or fingernail beds, indicating low oxygen levels.
- Confusion or difficulty concentrating, which may result from lack of oxygen to the brain.
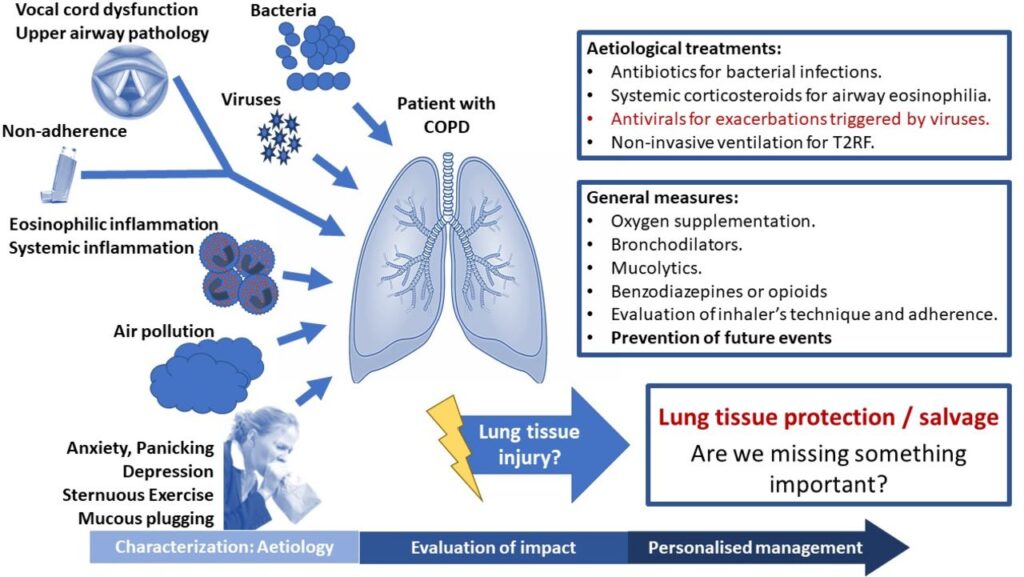
Care and Management Strategies
While there is no cure for this respiratory condition, several strategies can help manage symptoms, slow disease progression, and improve overall quality of life. A combination of lifestyle changes, medications, and therapies is often recommended.
Lifestyle Modifications
Making certain lifestyle changes can significantly reduce symptoms and prevent complications:
- Quit Smoking: Stopping smoking is the single most effective step to slow the progression of the disease. Support programs, counseling, and medications can aid in quitting.
- Avoid Irritants: Minimize exposure to air pollution, dust, and chemical fumes by using air purifiers, wearing masks, and ensuring proper ventilation in living spaces.
- Exercise Regularly: Engaging in light physical activity, such as walking or swimming, can strengthen respiratory muscles and improve endurance.
- Eat a Balanced Diet: Consuming nutrient-rich foods supports overall health and helps maintain a healthy weight, which is essential for managing symptoms.
Medications
Several medications are available to alleviate symptoms and reduce flare-ups:
- Bronchodilators: These medications relax the muscles around the airways, making it easier to breathe. They are often administered through inhalers.
- Inhaled Steroids: These reduce inflammation in the airways and are particularly helpful for individuals with frequent flare-ups.
- Antibiotics: Used to treat respiratory infections that can exacerbate symptoms.
Oxygen Therapy
For individuals with severe cases, supplemental oxygen may be necessary to maintain adequate oxygen levels in the blood. Portable oxygen devices allow patients to remain active while receiving the support they need.
Pulmonary Rehabilitation
Pulmonary rehabilitation programs combine exercise, education, and support to help individuals manage their condition effectively. These programs teach breathing techniques, provide nutritional guidance, and offer emotional support to improve overall well-being.
Vaccinations
Staying up-to-date with vaccinations is critical for preventing respiratory infections, which can worsen symptoms. Annual flu shots and pneumonia vaccines are highly recommended for individuals with this lung condition.
Living with Chronic Obstructive Pulmonary Disease
Managing this condition requires a proactive approach and ongoing commitment to self-care. By understanding the triggers and adopting healthy habits, individuals can lead fulfilling lives despite the challenges posed by the disease.
Building a Support Network
Connecting with others who share similar experiences can provide emotional support and practical advice. Support groups, both in-person and online, offer a platform to discuss concerns, share coping strategies, and celebrate successes.
Monitoring Progress
Regular check-ups with healthcare providers are essential for monitoring the disease’s progression and adjusting treatment plans as needed. Keeping track of symptoms and reporting any changes promptly can help prevent complications.
Planning for Emergencies
Having an action plan in place for flare-ups or emergencies can make a significant difference. This includes knowing when to use rescue medications, contacting healthcare providers, and seeking emergency care when necessary.