Chronic Kidney Failure, also known as End-Stage Renal Disease or ESRD, represents the final stage of chronic kidney disease. At this stage, the kidneys are no longer able to perform their essential functions effectively, necessitating medical intervention to sustain life. Understanding the condition, its symptoms, and how to manage it is crucial for patients, caregivers, and healthcare providers alike.
What is Chronic Kidney Failure?
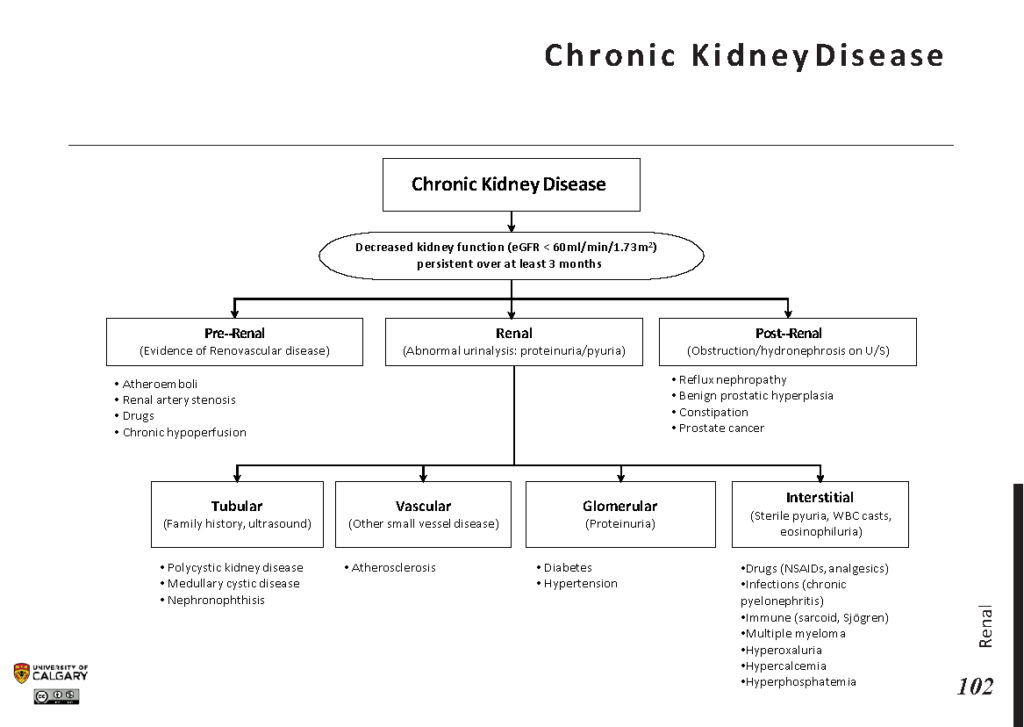
Chronic Kidney Failure occurs when the kidneys lose their ability to filter waste products, excess fluids, and toxins from the blood. This decline in kidney function is gradual and typically results from prolonged damage caused by conditions such as diabetes, high blood pressure, or other underlying health issues. When kidney function drops below a certain threshold—usually less than 15 percent of normal capacity—the condition is classified as end-stage kidney failure.
The kidneys play a vital role in maintaining overall health. They regulate electrolyte balance, control blood pressure, produce hormones that stimulate red blood cell production, and remove waste products from the body. When these organs fail, the entire body can be affected, leading to a cascade of complications.
Common Causes of Chronic Kidney Failure
- Diabetes: High blood sugar levels over time can damage the small blood vessels in the kidneys, impairing their function.
- Hypertension: Elevated blood pressure places stress on the kidneys, causing them to weaken over time.
- Glomerulonephritis: Inflammation of the kidney’s filtering units can lead to progressive damage.
- Polycystic Kidney Disease: A genetic disorder characterized by the growth of cysts in the kidneys, which can disrupt their function.
- Prolonged Use of Certain Medications: Overuse of pain relievers or other medications can harm the kidneys.
Symptoms of Chronic Kidney Failure
In the early stages of kidney disease, symptoms may be mild or even absent. However, as the condition progresses to end-stage kidney failure, the signs become more pronounced and debilitating. Recognizing these symptoms early can help individuals seek timely medical care and improve their quality of life.
Physical Symptoms
- Fatigue: Feeling constantly tired or weak is a common symptom due to the buildup of toxins in the body.
- Swelling: Fluid retention can cause swelling in the legs, ankles, feet, or face.
- Shortness of Breath: Excess fluid in the lungs or anemia can make breathing difficult.
- Nausea and Vomiting: The accumulation of waste products in the blood can lead to digestive issues.
- Changes in Urination: Patients may notice reduced urine output, foamy urine, or blood in the urine.
Emotional and Cognitive Symptoms
- Confusion: Toxins in the bloodstream can affect brain function, leading to confusion or difficulty concentrating.
- Mood Swings: Depression, anxiety, or irritability may arise due to the physical and emotional toll of the condition.
- Loss of Appetite: Many individuals experience a decreased desire to eat, which can contribute to weight loss and malnutrition.
Managing Chronic Kidney Failure
While there is no cure for end-stage kidney failure, several treatment options and lifestyle adjustments can help manage the condition and improve the patient’s quality of life. The choice of treatment depends on the individual’s overall health, preferences, and available resources.
Dialysis: A Lifeline for Many
Dialysis is a medical procedure that artificially removes waste products, excess fluids, and toxins from the blood when the kidneys can no longer do so. There are two primary types of dialysis:
Hemodialysis
Hemodialysis involves using a machine called a dialyzer to filter the blood outside the body. During the procedure, blood is removed from the body, passed through the dialyzer, and then returned to the bloodstream. Hemodialysis is typically performed at a dialysis center three times a week, although some patients may use home hemodialysis systems.
Peritoneal Dialysis
Peritoneal dialysis uses the lining of the abdomen, known as the peritoneum, as a natural filter. A special solution is introduced into the abdominal cavity through a catheter, allowing waste products and excess fluids to pass from the blood into the solution. The used solution is then drained and replaced with fresh solution. This type of dialysis can often be done at home, offering greater flexibility for patients.
Kidney Transplantation: A Long-Term Solution
A kidney transplant involves surgically replacing a failed kidney with a healthy one from a donor. The donor kidney can come from a living or deceased individual. While transplantation offers the potential for a more normal life without the need for dialysis, it requires lifelong use of immunosuppressive medications to prevent the body from rejecting the new organ.
Not all patients are eligible for a kidney transplant. Factors such as age, overall health, and the presence of other medical conditions can influence candidacy. Additionally, the availability of suitable donor kidneys can be a limiting factor.
Lifestyle Modifications
Beyond medical treatments, making certain lifestyle changes can significantly impact the management of chronic kidney failure. These modifications aim to reduce the strain on the kidneys and improve overall well-being.
Dietary Adjustments
- Limit Sodium Intake: Reducing salt consumption can help control blood pressure and minimize fluid retention.
- Monitor Protein Consumption: While protein is essential, excessive intake can strain the kidneys. A balanced approach is key.
- Restrict Potassium and Phosphorus: High levels of these minerals can be harmful to individuals with kidney failure.
- Stay Hydrated: Adequate fluid intake is important, but overhydration should be avoided.
Regular Exercise
Engaging in regular physical activity can improve cardiovascular health, boost energy levels, and enhance mood. Activities such as walking, swimming, or cycling are generally safe and beneficial for individuals with chronic kidney failure, provided they are approved by a healthcare provider.
Smoking Cessation and Alcohol Moderation
Smoking and excessive alcohol consumption can exacerbate kidney damage and worsen overall health. Quitting smoking and limiting alcohol intake are critical steps in managing the condition.
Emotional and Psychological Support
Living with chronic kidney failure can be emotionally challenging. Patients may experience feelings of frustration, fear, or isolation. Seeking support from mental health professionals, joining support groups, or connecting with others who share similar experiences can provide valuable emotional relief and practical advice.
Preventing Progression of Kidney Disease
For individuals with earlier stages of kidney disease, taking proactive steps can slow the progression of the condition and potentially delay the onset of end-stage kidney failure. Early intervention is key to preserving kidney function and improving long-term outcomes.
Control Underlying Conditions
Managing conditions such as diabetes and hypertension is crucial in preventing further kidney damage. Regular monitoring, adherence to prescribed medications, and lifestyle changes can help keep these conditions under control.
Regular Medical Check-Ups
Frequent visits to a healthcare provider allow for ongoing assessment of kidney function and early detection of any changes. Blood tests, urine tests, and imaging studies are commonly used to evaluate kidney health.
Educate Yourself and Advocate for Your Health
Understanding your condition empowers you to make informed decisions about your care. Asking questions, staying informed about treatment options, and actively participating in your healthcare plan can make a significant difference in managing chronic kidney failure.