Charcot foot, also known as neuropathic arthropathy, is a serious condition that affects the bones, joints, and soft tissues of the foot. It often occurs in individuals with significant nerve damage, particularly those with diabetes. This condition can lead to severe deformities, instability, and even amputation if not managed properly. Understanding its causes, symptoms, and treatment options is crucial for both patients and healthcare providers. In this article, we will explore Charcot foot in detail, shedding light on its underlying mechanisms, risk factors, and strategies for effective management.
What is Charcot Foot?
Charcot foot is a progressive condition characterized by the weakening of bones in the foot due to nerve damage. The condition was first described by Jean-Martin Charcot in the late 19th century, and it primarily affects individuals with conditions such as diabetes, spinal cord injuries, or other diseases that cause peripheral neuropathy. The hallmark of Charcot foot is the breakdown of bone and joint structures, leading to deformities and loss of function.
The condition typically begins with inflammation in the affected area, followed by gradual destruction of the bones and joints. Without proper intervention, the foot may become misshapen, making walking difficult and increasing the risk of ulcers and infections.
Causes of Charcot Foot
Several factors contribute to the development of Charcot foot. Below are the primary causes:
Peripheral Neuropathy
Peripheral neuropathy is one of the most common underlying causes of Charcot foot. This condition involves damage to the nerves in the feet, often due to diabetes. When the nerves are damaged, individuals lose sensation in their feet, making them unaware of injuries or repetitive stress. Over time, this lack of sensation can lead to fractures or dislocations that go unnoticed and untreated.
Trauma
Even minor trauma can trigger Charcot foot in individuals with pre-existing nerve damage. For example, a small sprain or repetitive pressure on the foot can initiate the inflammatory process that leads to bone and joint destruction. Because people with neuropathy may not feel pain, they continue to walk on the injured foot, exacerbating the damage.
Inflammation
Inflammation plays a critical role in the progression of Charcot foot. When the body detects an injury, it responds by sending inflammatory cells to the affected area. However, in individuals with neuropathy, this inflammatory response can become excessive and prolonged, leading to further destruction of bone and joint tissue.
Blood Flow Changes
Poor circulation is another contributing factor. Conditions like diabetes can impair blood flow to the extremities, reducing the delivery of oxygen and nutrients necessary for healing. As a result, bones and tissues in the foot become more vulnerable to damage and slower to repair themselves.
Symptoms of Charcot Foot
Recognizing the symptoms of Charcot foot early is essential for preventing complications. Some of the most common signs include:
- Swelling: The affected foot may appear swollen, even without any obvious injury.
- Redness: The skin over the affected area may become red and warm to the touch.
- Deformity: Over time, the foot may develop noticeable deformities, such as a collapsed arch or a “rocker-bottom” appearance.
- Pain: While many individuals with neuropathy do not experience pain, some may notice mild discomfort or soreness in the early stages.
- Instability: The foot may feel unstable or weak, making it difficult to walk.
Diagnosis of Charcot Foot
Diagnosing Charcot foot requires a thorough evaluation by a healthcare professional. The process typically includes:
Clinical Examination
A physical examination is the first step in diagnosing the condition. The doctor will assess the foot for signs of swelling, redness, warmth, and deformity. They may also check for areas of tenderness or instability.
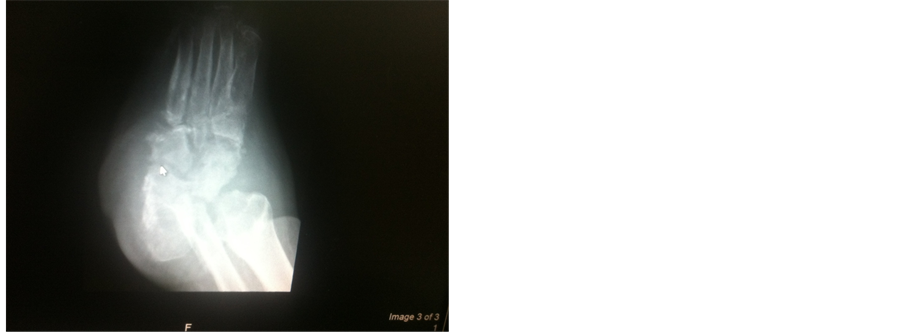
Imaging Tests
X-rays are commonly used to evaluate bone and joint abnormalities. In the early stages of Charcot foot, X-rays may show subtle changes, such as small fractures or joint dislocations. As the condition progresses, more severe deformities may become apparent. Advanced imaging techniques, such as magnetic resonance imaging or computed tomography scans, may be used to provide a more detailed view of the affected area.
Laboratory Tests
Blood tests may be performed to rule out infections or other systemic conditions that could mimic the symptoms of Charcot foot. For example, elevated white blood cell counts or markers of inflammation may indicate an infection rather than neuropathic arthropathy.
Management of Charcot Foot
Managing Charcot foot requires a multidisciplinary approach, involving podiatrists, orthopedic specialists, and other healthcare professionals. Treatment focuses on stabilizing the foot, preventing further damage, and addressing any underlying conditions. Below are the key components of management:
Immobilization
One of the primary goals of treatment is to immobilize the foot to allow healing. This is typically achieved through the use of casts, braces, or specialized boots. Immobilization helps reduce stress on the bones and joints, preventing further damage. In some cases, patients may need to use crutches or wheelchairs to avoid putting weight on the affected foot.
Custom Orthotics
Once the acute phase has resolved, custom orthotic devices may be prescribed to support the foot and prevent recurrence. These devices are designed to redistribute pressure and stabilize the foot during walking.
Surgery
In severe cases, surgery may be necessary to correct deformities or repair damaged bones and joints. Surgical options include realigning bones, fusing joints, or removing damaged tissue. Surgery is typically considered only when conservative measures have failed or when there is a high risk of complications, such as ulcers or infections.
Management of Underlying Conditions
Addressing the underlying cause of Charcot foot is essential for long-term management. For individuals with diabetes, maintaining good blood sugar control is critical to slowing the progression of nerve damage. Regular monitoring of blood glucose levels, adherence to a healthy diet, and appropriate medication can help reduce the risk of complications.
Regular Monitoring
Patients with Charcot foot require ongoing monitoring to detect any changes in the condition of their feet. Regular visits to a podiatrist or foot specialist are recommended to ensure early intervention if new issues arise.
Prevention of Charcot Foot
While Charcot foot cannot always be prevented, certain measures can reduce the risk of developing the condition:
- Foot Care: Individuals with neuropathy should inspect their feet daily for signs of injury, redness, or swelling. Proper hygiene and moisturizing can help maintain skin integrity.
- Footwear: Wearing well-fitting, supportive shoes can help reduce stress on the feet. Avoiding high heels or poorly cushioned shoes is especially important.
- Weight Management: Maintaining a healthy weight can reduce pressure on the feet and lower the risk of fractures or deformities.
- Regular Check-Ups: Routine visits to a healthcare provider can help identify early signs of nerve damage or foot problems.
Living with Charcot Foot
Living with Charcot foot can be challenging, but with proper care and management, individuals can maintain mobility and quality of life. Education is a key component of living with the condition. Patients should be aware of the importance of foot care, regular monitoring, and adherence to treatment plans. Support from family, friends, and healthcare providers can also play a vital role in helping individuals cope with the physical and emotional challenges associated with the condition.