Cellulitis, often abbreviated as CE, is a common yet potentially serious bacterial skin infection. It can affect individuals of all ages and requires prompt medical attention to prevent complications. This article explores the causes, symptoms, and treatment options for cellulitis in detail, offering valuable insights into managing this condition effectively.

Understanding Cellulitis
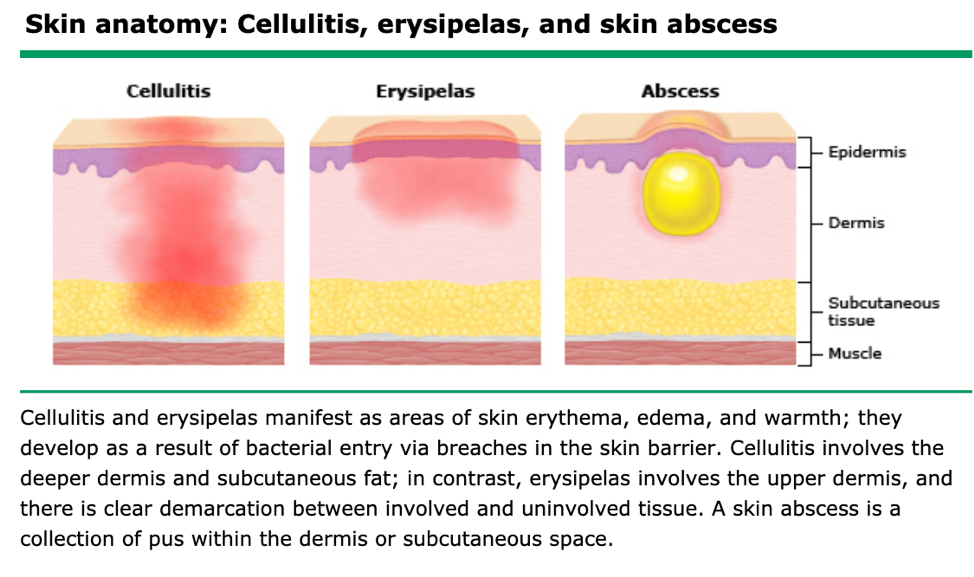
Cellulitis is a bacterial infection that affects the deeper layers of the skin, including the dermis and subcutaneous tissues. Unlike superficial infections that only impact the outermost layer of the skin, cellulitis penetrates deeper, leading to inflammation and other systemic symptoms. Understanding its nature is crucial for early detection and treatment.
How Does Cellulitis Develop?
The development of cellulitis typically begins when bacteria enter the body through a break in the skin. These breaks can be caused by cuts, scrapes, insect bites, surgical wounds, or even conditions like eczema or athlete’s foot that compromise the skin’s integrity. Once inside, the bacteria multiply and trigger an immune response, resulting in redness, swelling, and pain.
Common Causes of Cellulitis
Several types of bacteria can cause cellulitis, with some being more prevalent than others. Below are the primary culprits behind this infection:
Streptococcus Bacteria
- Streptococcus bacteria are among the most common causes of cellulitis. These bacteria thrive in warm, moist environments and can easily spread from person to person.
- Group A Streptococcus is particularly notorious for causing severe cases of cellulitis.
Staphylococcus Bacteria
- Staphylococcus bacteria, especially Staphylococcus aureus, are another leading cause of cellulitis.
- These bacteria are commonly found on the skin and in the nasal passages of healthy individuals but can become problematic when they enter the body through a wound.
Other Potential Causes
- In rare cases, cellulitis can be caused by other bacteria such as Haemophilus influenzae or Pasteurella multocida.
- Individuals with weakened immune systems may be susceptible to cellulitis caused by less common pathogens.
Symptoms of Cellulitis
Recognizing the symptoms of cellulitis is essential for timely intervention. The signs and symptoms can vary depending on the severity of the infection and the area affected. Here are the most common manifestations:
Localized Symptoms
- Redness: The affected area often appears red and inflamed. The redness may expand over time.
- Swelling: Swelling is a hallmark symptom of cellulitis and is usually accompanied by tenderness.
- Pain: The infected area is typically painful to the touch and may feel warm.
- Blistering: In some cases, small blisters or pus-filled bumps may form on the skin.
Systemic Symptoms
- Fever: Many individuals with cellulitis experience a fever, which indicates that the infection has triggered a systemic immune response.
- Chills: Chills often accompany fever and are a sign that the body is fighting off the infection.
- Fatigue: Generalized tiredness and malaise are common in more severe cases of cellulitis.
When to Seek Medical Attention
While mild cases of cellulitis can sometimes resolve with home care, certain symptoms warrant immediate medical attention. These include:
- Rapidly spreading redness or swelling
- High fever or chills
- Nausea or vomiting
- Confusion or dizziness
Risk Factors for Developing Cellulitis
Certain factors increase the likelihood of developing cellulitis. Being aware of these risk factors can help individuals take preventive measures.
Preexisting Skin Conditions
- Conditions like eczema, psoriasis, and fungal infections create openings in the skin that make it easier for bacteria to enter.
- Athlete’s foot and other chronic skin issues should be treated promptly to reduce the risk of cellulitis.
Weakened Immune System
- Individuals with diabetes, HIV/AIDS, or cancer are at higher risk because their immune systems are compromised.
- Medications that suppress the immune system, such as corticosteroids, can also increase susceptibility.
Obesity
- Excess weight can put additional strain on the lymphatic system, making it harder for the body to fight infections.
- Obesity is also associated with poor circulation, which can slow down the healing process.
Treatment Options for Cellulitis
Treatment for cellulitis focuses on eliminating the infection, relieving symptoms, and preventing complications. The approach may vary depending on the severity of the condition.
Antibiotics
- Oral antibiotics are the first line of treatment for most cases of cellulitis. Commonly prescribed antibiotics include penicillin, amoxicillin, and cephalosporins.
- In severe cases, intravenous antibiotics may be administered in a hospital setting to ensure faster delivery of the medication.
Pain Management
- Over-the-counter pain relievers like acetaminophen or ibuprofen can help manage discomfort and reduce inflammation.
- Applying a cool compress to the affected area may also provide temporary relief.
Elevation and Rest
- Elevating the affected limb can reduce swelling and improve blood flow, aiding in the healing process.
- Avoiding strenuous activities allows the body to focus its energy on fighting the infection.
Wound Care
- If cellulitis developed due to an open wound, proper cleaning and dressing of the wound are essential to prevent further infection.
- Regularly changing bandages and keeping the area dry can promote faster healing.
Preventing Cellulitis
While it may not always be possible to prevent cellulitis, certain measures can significantly reduce the risk of developing this infection.
Proper Wound Care
- Clean all cuts, scrapes, and wounds immediately with soap and water.
- Apply an antiseptic ointment and cover the area with a sterile bandage.
Maintaining Good Hygiene
- Regular handwashing and keeping the skin clean and moisturized can help prevent infections.
- Avoid sharing personal items like razors or towels, which can harbor bacteria.
Managing Chronic Conditions
- Individuals with diabetes should monitor their blood sugar levels closely and inspect their feet daily for signs of injury.
- Treating underlying skin conditions like eczema or athlete’s foot promptly can reduce the risk of cellulitis.
Complications of Untreated Cellulitis
If left untreated, cellulitis can lead to serious complications that extend beyond the skin. Some of these complications include:
Spread of Infection
- The infection can spread to nearby tissues, bones, or the bloodstream, leading to life-threatening conditions like sepsis.
- Lymphangitis, an infection of the lymph vessels, is another potential complication.
Permanent Damage
- Severe cases of cellulitis can result in permanent scarring or changes in skin texture.
- Recurrent cellulitis may damage the lymphatic system, causing chronic swelling known as lymphedema.
Impact on Quality of Life
- Prolonged or recurrent cellulitis can interfere with daily activities and reduce overall quality of life.
- Emotional stress and anxiety may arise from dealing with persistent infections.