Carotid artery disease, also known as CAD, is a serious medical condition that affects the blood vessels in the neck responsible for supplying oxygen-rich blood to the brain. This condition occurs when these arteries become narrowed or blocked due to the buildup of fatty deposits, known as plaque. If left untreated, carotid artery disease can lead to severe complications, including stroke. In this article, we will explore the causes, symptoms, and treatment options available for this condition.
Understanding Carotid Artery Disease
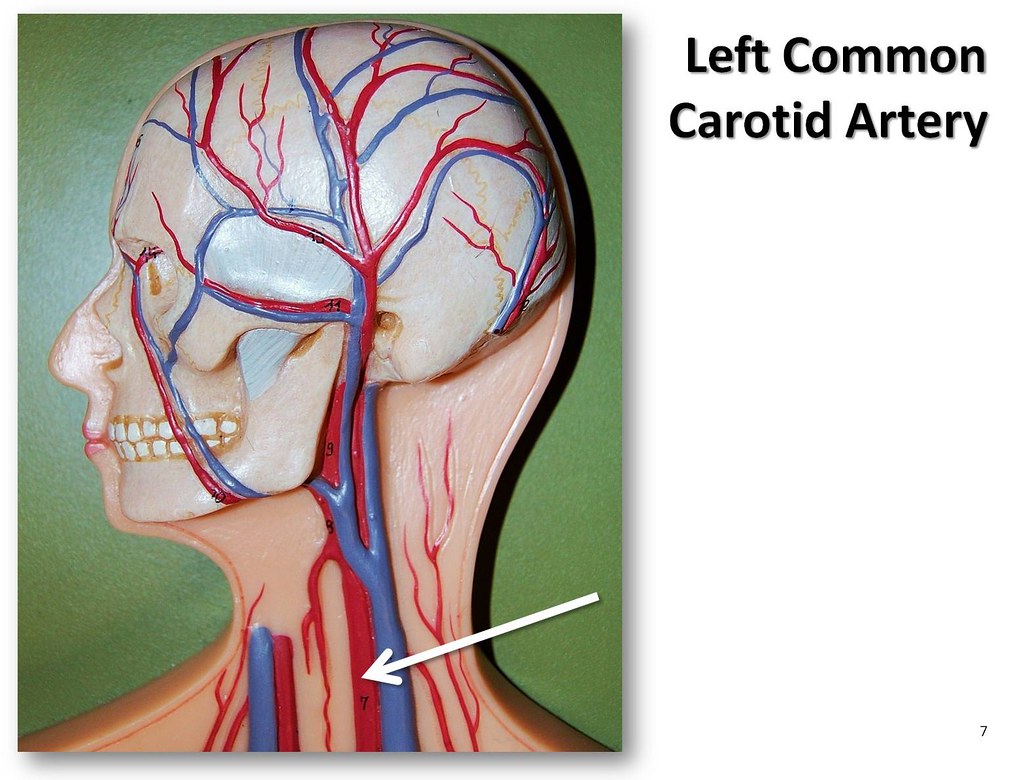
The carotid arteries are two large blood vessels located on either side of the neck. Their primary function is to deliver oxygenated blood from the heart to the brain. When these arteries become narrowed, it disrupts the flow of blood, increasing the risk of a stroke. The narrowing is typically caused by a process called atherosclerosis, which involves the accumulation of plaque inside the arterial walls.
What Happens During Atherosclerosis?
Atherosclerosis begins when cholesterol, fat, calcium, and other substances circulating in the blood start to accumulate on the inner walls of the arteries. Over time, these deposits harden and narrow the arteries, restricting blood flow. The plaque can also break loose, forming clots that may travel to the brain and cause a blockage, leading to a stroke.
Causes of Carotid Artery Disease
Several factors contribute to the development of carotid artery disease. Understanding these causes can help individuals take preventive measures to reduce their risk.
Unhealthy Lifestyle Choices
- Poor Diet: Consuming foods high in saturated fats, trans fats, and cholesterol can increase the levels of bad cholesterol in the blood, contributing to plaque buildup.
- Lack of Physical Activity: A sedentary lifestyle can lead to weight gain, high blood pressure, and poor circulation, all of which increase the risk of developing carotid artery disease.
- Smoking: Smoking damages the lining of the arteries, making it easier for plaque to adhere to the walls. It also reduces the amount of oxygen in the blood, further straining the cardiovascular system.
Medical Conditions
- High Blood Pressure: Elevated blood pressure puts extra stress on the arteries, causing them to weaken and become more susceptible to plaque buildup.
- Diabetes: People with diabetes often have high levels of glucose in their blood, which can damage blood vessels and accelerate the progression of atherosclerosis.
- High Cholesterol: Excessive levels of low-density lipoprotein, commonly referred to as bad cholesterol, contribute to the formation of plaque in the arteries.
Genetic Factors
Some individuals may be predisposed to carotid artery disease due to their family history. If close relatives have experienced heart disease or strokes, there may be an increased likelihood of developing similar conditions.
Symptoms of Carotid Artery Disease
In its early stages, carotid artery disease often does not produce noticeable symptoms. However, as the condition progresses and blood flow to the brain becomes significantly restricted, certain warning signs may appear. These symptoms should not be ignored, as they could indicate an impending stroke.
Transient Ischemic Attacks
Transient ischemic attacks, sometimes referred to as mini-strokes, are temporary episodes caused by a brief reduction in blood supply to the brain. Although they do not cause permanent damage, they serve as a critical warning sign of underlying carotid artery disease. Common symptoms include:
- Sudden numbness or weakness, particularly on one side of the body
- Difficulty speaking or understanding speech
- Blurred or loss of vision in one or both eyes
- Dizziness or loss of balance
- Severe headaches with no apparent cause
Warning Signs of an Impending Stroke
If carotid artery disease is left untreated, it can lead to a full-blown stroke. Recognizing the symptoms of a stroke is crucial for seeking immediate medical attention. Key indicators include:
- Sudden confusion or trouble speaking
- Paralysis or weakness in the face, arm, or leg
- Trouble walking or maintaining balance
- Severe headache with no known cause
Diagnosis of Carotid Artery Disease
To diagnose carotid artery disease, healthcare providers use a combination of physical examinations, imaging tests, and laboratory analyses. Early detection is essential for preventing complications such as stroke.
Physical Examination
During a routine checkup, a doctor may listen to the carotid arteries using a stethoscope. An abnormal sound, known as a bruit, may indicate turbulent blood flow caused by narrowing of the arteries.
Imaging Tests
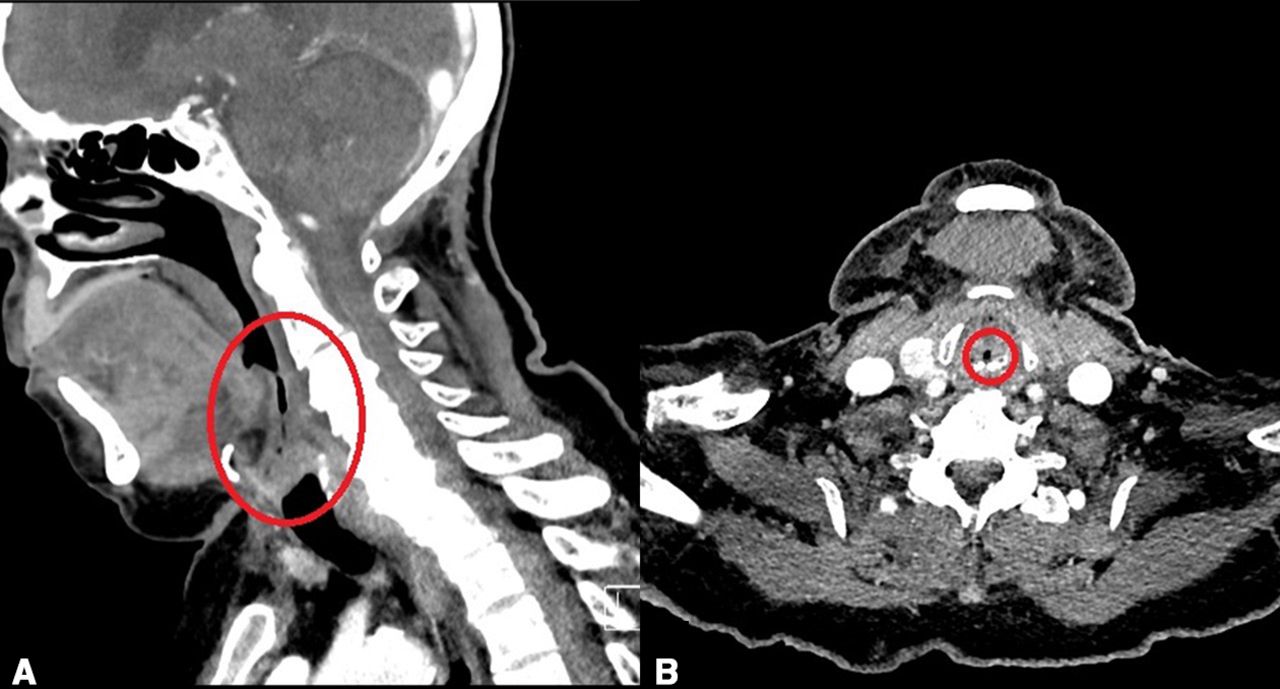
- Carotid Ultrasound: This non-invasive test uses sound waves to create images of the carotid arteries, allowing doctors to assess the extent of narrowing.
- Magnetic Resonance Imaging: MRI scans provide detailed images of the arteries and surrounding tissues, helping to identify areas of blockage.
- Computed Tomography Angiography: This imaging technique combines X-rays and computer technology to produce cross-sectional images of the arteries.
Blood Tests
Blood tests may be conducted to measure cholesterol levels, blood sugar, and other markers that can indicate an increased risk of carotid artery disease.
Treatment Options for Carotid Artery Disease
The treatment of carotid artery disease focuses on reducing the risk of stroke and improving overall cardiovascular health. Treatment plans are tailored to the severity of the condition and the individual’s overall health.
Lifestyle Modifications
Adopting healthier habits is often the first step in managing carotid artery disease. These changes can slow the progression of the disease and improve quality of life.
- Dietary Changes: Eating a balanced diet rich in fruits, vegetables, whole grains, and lean proteins can help lower cholesterol and blood pressure.
- Regular Exercise: Engaging in moderate physical activity, such as walking or swimming, can improve circulation and strengthen the heart.
- Quitting Smoking: Eliminating tobacco use is one of the most effective ways to reduce the risk of complications.
Medications
Doctors may prescribe medications to manage underlying conditions and prevent further narrowing of the arteries.
- Cholesterol-Lowering Drugs: Statins are commonly prescribed to reduce levels of bad cholesterol and stabilize plaque in the arteries.
- Blood Pressure Medications: Antihypertensive drugs help control high blood pressure, reducing strain on the arteries.
- Antiplatelet Medications: Aspirin or other antiplatelet drugs can prevent blood clots from forming, lowering the risk of stroke.
Surgical Interventions
In cases where the arteries are severely narrowed, surgical procedures may be necessary to restore proper blood flow.
- Carotid Endarterectomy: This procedure involves surgically removing plaque from the carotid arteries to improve blood flow.
- Carotid Artery Stenting: A stent, or small mesh tube, is inserted into the artery to keep it open and allow blood to flow freely.
Preventing Carotid Artery Disease
While some risk factors, such as age and genetics, cannot be changed, many preventive measures can significantly reduce the likelihood of developing carotid artery disease.
Healthy Habits
- Maintain a healthy weight through a balanced diet and regular exercise.
- Monitor and manage chronic conditions like diabetes and hypertension.
- Avoid smoking and limit alcohol consumption.
Regular Medical Checkups
Scheduling routine visits with a healthcare provider allows for early detection of risk factors and timely intervention. Blood pressure, cholesterol levels, and other key indicators should be monitored regularly.
Education and Awareness
Raising awareness about the signs and symptoms of carotid artery disease can empower individuals to seek medical attention promptly. Understanding the importance of preventive care is key to maintaining long-term cardiovascular health.