Cardiac tamponade, often abbreviated as CT, is a life-threatening medical condition that occurs when fluid accumulates in the pericardium, the protective sac surrounding the heart. This buildup of fluid compresses the heart, preventing it from functioning properly and leading to potentially fatal consequences if not treated promptly. Cardiac tamponade is closely associated with pericardial effusion, which refers to the abnormal accumulation of fluid within the pericardial space. In this article, we will explore the causes, symptoms, diagnosis, and treatment options for cardiac tamponade, shedding light on this critical cardiovascular condition.
What is Cardiac Tamponade?
Cardiac tamponade is a serious condition where excessive fluid in the pericardium exerts pressure on the heart, impairing its ability to pump blood effectively. The heart is enclosed in a double-layered sac called the pericardium, which normally contains a small amount of lubricating fluid to reduce friction during heartbeats. However, when an abnormal amount of fluid accumulates in this space, it can compress the heart chambers, particularly the atria and ventricles, restricting their ability to fill with blood. This results in reduced cardiac output and compromised circulation throughout the body.
The Role of the Pericardium
The pericardium serves as a protective barrier for the heart, shielding it from infections and providing structural support. It also helps maintain the heart’s position within the chest cavity. While a small amount of fluid in the pericardial space is normal, any significant increase can lead to complications. When fluid accumulation becomes excessive, it can interfere with the heart’s pumping action, leading to cardiac tamponade.
Causes of Cardiac Tamponade
There are several potential causes of cardiac tamponade, ranging from traumatic injuries to underlying medical conditions. Understanding these causes is essential for early detection and effective management of the condition.
Trauma or Injury
- Chest Trauma: Blunt or penetrating injuries to the chest can damage the pericardium, leading to bleeding and fluid accumulation.
- Surgical Complications: Certain heart surgeries or invasive procedures, such as catheter-based interventions, can inadvertently cause bleeding into the pericardial space.
Infections
- Viral Infections: Viral pericarditis, an inflammation of the pericardium, can result in fluid buildup.
- Bacterial Infections: Severe bacterial infections, including tuberculosis, can lead to purulent pericarditis, causing significant fluid accumulation.
Cancer
- Malignant Tumors: Cancerous growths in the pericardium or nearby structures can invade the pericardial space, leading to fluid production.
- Metastatic Disease: Cancers such as lung cancer or breast cancer can spread to the pericardium, resulting in malignant effusions.
Autoimmune Disorders
- Lupus: Systemic lupus erythematosus can cause inflammation of the pericardium, leading to fluid accumulation.
- Rheumatoid Arthritis: Chronic inflammatory conditions like rheumatoid arthritis can also contribute to pericardial effusion.
Other Causes
- Kidney Failure: Impaired kidney function can lead to fluid retention, increasing the risk of pericardial effusion.
- Hypothyroidism: Severe underactive thyroid can cause myxedema, a condition associated with fluid accumulation in various parts of the body, including the pericardium.
Symptoms of Cardiac Tamponade
The symptoms of cardiac tamponade often develop rapidly and can vary depending on the severity of the condition. Early recognition of these symptoms is crucial for timely intervention.
Classic Triad of Symptoms
Cardiac tamponade is often characterized by a classic triad of symptoms, although not all patients may exhibit all three:
- Low Blood Pressure: Reduced cardiac output leads to hypotension, or abnormally low blood pressure.
- Increased Heart Rate: The heart compensates for reduced pumping efficiency by beating faster, resulting in tachycardia.
- Jugular Vein Distention: Elevated pressure in the veins of the neck, known as jugular venous distention, is a hallmark sign of impaired heart filling.
Additional Symptoms
- Chest Pain: Patients may experience sharp or stabbing chest pain that worsens with deep breaths or lying down.
- Shortness of Breath: Difficulty breathing, especially when lying flat, is a common symptom due to reduced cardiac output.
- Fatigue and Weakness: Decreased blood flow to tissues can cause extreme tiredness and weakness.
- Dizziness or Fainting: Reduced blood flow to the brain can lead to lightheadedness or loss of consciousness.
Diagnosis of Cardiac Tamponade
Diagnosing cardiac tamponade requires a combination of clinical evaluation, imaging studies, and laboratory tests. Early and accurate diagnosis is critical to prevent complications.
Physical Examination
A thorough physical examination is the first step in diagnosing cardiac tamponade. Physicians look for signs such as jugular vein distention, muffled heart sounds, and low blood pressure. These findings, combined with the patient’s medical history, can raise suspicion of the condition.
Imaging Studies
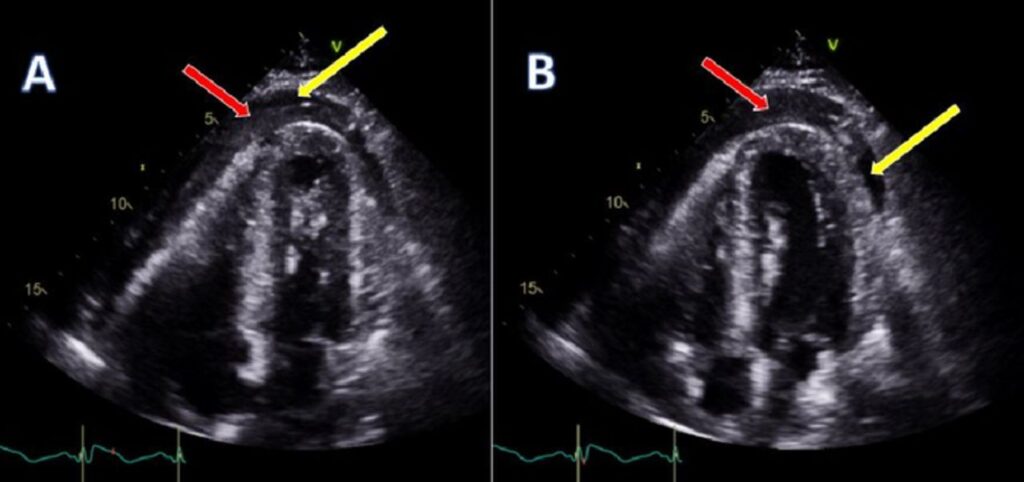
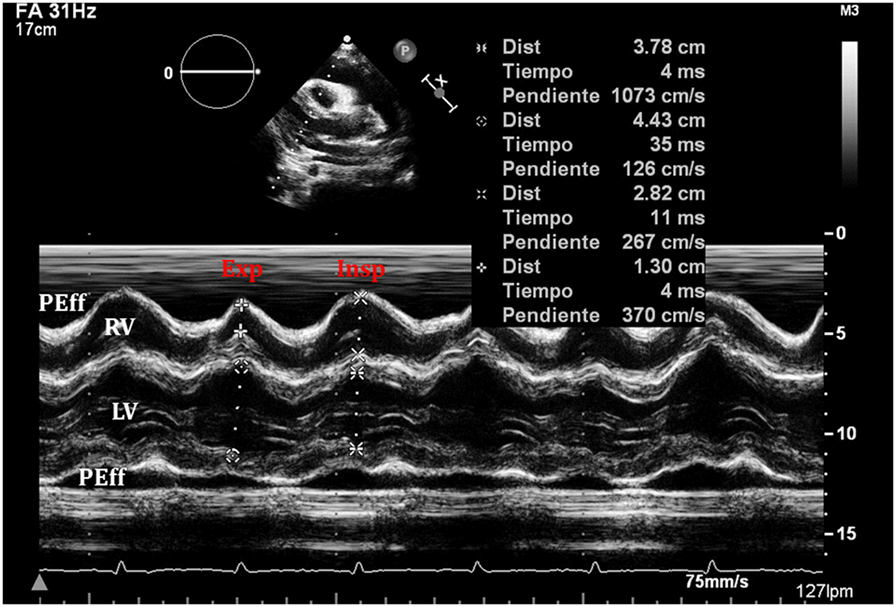
- Echocardiogram: This non-invasive ultrasound test is the gold standard for diagnosing cardiac tamponade. It provides detailed images of the heart and pericardium, allowing doctors to assess fluid accumulation and its impact on heart function.
- Chest X-ray: A chest X-ray may reveal an enlarged cardiac silhouette, indicating fluid buildup around the heart.
- Computed Tomography (CT) Scan: CT scans can provide additional information about the extent of fluid accumulation and identify potential causes, such as tumors or infections.
Laboratory Tests
- Blood Tests: Blood work can help identify underlying causes, such as infections or autoimmune disorders.
- Pericardial Fluid Analysis: If fluid is drained from the pericardium, it can be analyzed to determine its composition and identify infectious or malignant causes.
Treatment Options for Cardiac Tamponade
Treatment for cardiac tamponade focuses on relieving pressure on the heart and addressing the underlying cause of fluid accumulation. Prompt intervention is essential to prevent life-threatening complications.
Emergency Interventions
- Pericardiocentesis: This procedure involves inserting a needle into the pericardial space to drain excess fluid. It provides immediate relief and is often performed in emergency settings.
- Pericardial Window: In cases where pericardiocentesis is insufficient or recurrent effusions occur, a surgical procedure called a pericardial window may be performed to create a permanent opening for fluid drainage.
Addressing Underlying Causes
- Antibiotics: If an infection is the cause, antibiotics or antiviral medications may be prescribed to treat the underlying condition.
- Anti-inflammatory Medications: Nonsteroidal anti-inflammatory drugs or corticosteroids may be used to reduce inflammation in cases of autoimmune-related pericarditis.
- Cancer Treatments: For malignant effusions, treatments such as chemotherapy or radiation therapy may be necessary to manage the underlying cancer.
Supportive Care
- Oxygen Therapy: Supplemental oxygen may be provided to improve oxygenation in patients with breathing difficulties.
- Inotropic Agents: Medications that enhance heart contractility may be administered to support cardiac function temporarily.
Prevention and Monitoring
While it may not always be possible to prevent cardiac tamponade, certain measures can reduce the risk of developing the condition or experiencing recurrence.
Regular Medical Checkups
Patients with a history of pericardial effusion or underlying conditions such as autoimmune disorders or cancer should undergo regular monitoring to detect early signs of fluid accumulation.
Managing Risk Factors
- Treating Infections Promptly: Early treatment of infections can prevent complications such as pericarditis.
- Controlling Chronic Conditions: Managing conditions like kidney failure, hypothyroidism, or autoimmune diseases can reduce the risk of pericardial effusion.
Post-Treatment Follow-Up
After treatment for cardiac tamponade, ongoing follow-up care is essential to monitor for recurrence and ensure optimal heart function. Regular echocardiograms and consultations with a cardiologist can help track progress and address any emerging issues.