Calciphylaxis, also known as Calcific Uremic Arteriolopathy or CUA, is a rare and life-threatening condition that primarily affects individuals with chronic kidney disease. This guide aims to provide a comprehensive overview of this complex disorder, covering its causes, symptoms, diagnosis, treatment options, and ongoing research efforts.
Understanding the Condition
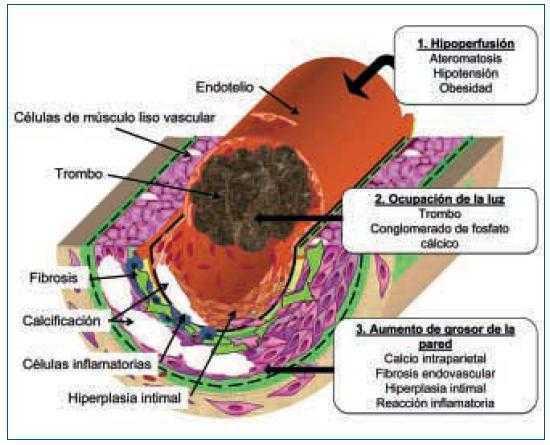
Calciphylaxis is a severe medical condition characterized by the abnormal deposition of calcium in the walls of small blood vessels, leading to tissue damage and skin ulcerations. While it predominantly occurs in people with advanced kidney disease, it can also affect individuals without kidney issues, albeit less commonly. The exact cause of this condition remains unclear, but several risk factors have been identified.
Risk Factors
- Chronic Kidney Disease: Most cases are observed in patients undergoing dialysis or those with end-stage renal disease.
- Hyperparathyroidism: Overactive parathyroid glands can contribute to abnormal calcium metabolism.
- Obesity: Excess body weight has been linked to an increased risk of developing calciphylaxis.
- Diabetes: Individuals with diabetes are at a higher risk due to associated vascular complications.
- Use of Certain Medications: Drugs such as warfarin and corticosteroids may increase susceptibility.
Symptoms and Clinical Presentation
The symptoms of calciphylaxis often manifest on the skin and can vary depending on the severity of the condition. Early recognition of these signs is crucial for timely intervention.
Common Symptoms
- Painful Skin Lesions: These typically appear as purplish or reddish nodules that progress to ulcers.
- Necrosis: Areas of dead tissue may develop, particularly in fatty regions like the thighs, abdomen, and buttocks.
- Infections: Open sores can become infected, leading to further complications.
- Systemic Symptoms: Some patients may experience fever, malaise, or other systemic signs of infection.
Diagnosis of Calciphylaxis
Diagnosing calciphylaxis requires a combination of clinical evaluation, laboratory tests, and imaging studies. Due to its rarity and nonspecific symptoms, misdiagnosis is common, making accurate identification challenging.
Clinical Evaluation
A thorough physical examination is essential to assess the appearance and distribution of skin lesions. Physicians will look for characteristic findings such as indurated plaques, retiform purpura, and necrotic ulcers.
Laboratory Tests
- Blood Tests: These include measurements of serum calcium, phosphorus, and parathyroid hormone levels to evaluate mineral metabolism.
- Biopsy: A skin biopsy is often performed to confirm the presence of calcium deposits in blood vessel walls, although this procedure carries risks of worsening the condition.
Imaging Studies
- X-rays: Can reveal calcifications in soft tissues and blood vessels.
- Doppler Ultrasound: Useful for assessing blood flow and detecting vascular abnormalities.
- CT Scans: Provide detailed images of calcified areas within the body.
Treatment Approaches
Managing calciphylaxis involves a multidisciplinary approach aimed at addressing underlying causes, alleviating symptoms, and preventing complications. Treatment strategies are tailored to individual patient needs and may evolve over time.
Medical Management
- Wound Care: Proper cleaning and dressing of ulcers are critical to prevent infections and promote healing.
- Pain Control: Effective pain management is necessary to improve quality of life.
- Antibiotics: Prescribed when there is evidence of infection in affected areas.
- Hyperbaric Oxygen Therapy: Sometimes used to enhance wound healing by increasing oxygen supply to damaged tissues.
Addressing Underlying Conditions
- Optimizing Dialysis: Ensuring adequate dialysis sessions to manage electrolyte imbalances.
- Parathyroidectomy: Surgical removal of overactive parathyroid glands may be considered in some cases.
- Medication Adjustments: Reviewing and modifying medications that could exacerbate the condition.
Emerging Therapies
Research into new treatments continues, with promising developments in pharmacological interventions and surgical techniques. Sodium thiosulfate, for example, has shown potential benefits in reducing calcium deposits and improving outcomes.
Ongoing Research and Future Directions
Despite advances in understanding calciphylaxis, much remains unknown about its pathophysiology and optimal management strategies. Ongoing research focuses on identifying biomarkers for early detection, exploring novel therapeutic agents, and refining existing treatment protocols.
Genetic Studies
Investigations into genetic predispositions aim to uncover hereditary factors that might influence susceptibility to calciphylaxis. Understanding these elements could pave the way for personalized medicine approaches.
Regenerative Medicine
Advances in regenerative medicine hold promise for repairing damaged tissues and restoring normal function. Techniques such as stem cell therapy and tissue engineering are being explored for their potential applications in treating calciphylaxis.
Clinical Trials
Participation in clinical trials offers hope for patients seeking innovative treatments. These studies evaluate the safety and efficacy of experimental drugs and procedures, contributing valuable data to the scientific community.
Living with Calciphylaxis
For those diagnosed with calciphylaxis, managing the condition extends beyond medical interventions. Lifestyle modifications, psychological support, and education play vital roles in coping with the challenges posed by this debilitating illness.
Lifestyle Modifications
- Dietary Changes: Adopting a balanced diet low in phosphorus and high in nutrients supports overall health.
- Exercise: Gentle physical activity helps maintain mobility and reduces the risk of complications.
- Smoking Cessation: Quitting smoking improves circulation and aids in healing processes.
Psychological Support
Dealing with chronic pain and visible skin changes can take a toll on mental well-being. Access to counseling services, support groups, and mental health professionals ensures comprehensive care for patients and their families.
Educational Resources
Empowering patients with knowledge about their condition enables them to make informed decisions regarding their healthcare. Educational materials, workshops, and online forums provide platforms for learning and sharing experiences.