Bullous pemphigoid, often abbreviated as BP, is a rare autoimmune skin condition that primarily affects older adults. This chronic disorder is characterized by the formation of large, fluid-filled blisters on the skin. While it may sound alarming, understanding its causes, recognizing its symptoms, undergoing proper diagnosis, and exploring treatment options can help manage this condition effectively. In this article, we will delve into the details of bullous pemphigoid to provide a comprehensive overview.
What is Bullous Pemphigoid?
Bullous pemphigoid is an autoimmune disease where the immune system mistakenly attacks a thin layer of tissue beneath the outer layer of the skin. This results in the formation of blisters that are typically large, tense, and filled with clear fluid. The condition most commonly affects individuals over the age of sixty, though it can occur at any age. It tends to develop slowly and can persist for months or even years if left untreated.
Understanding Autoimmune Disorders
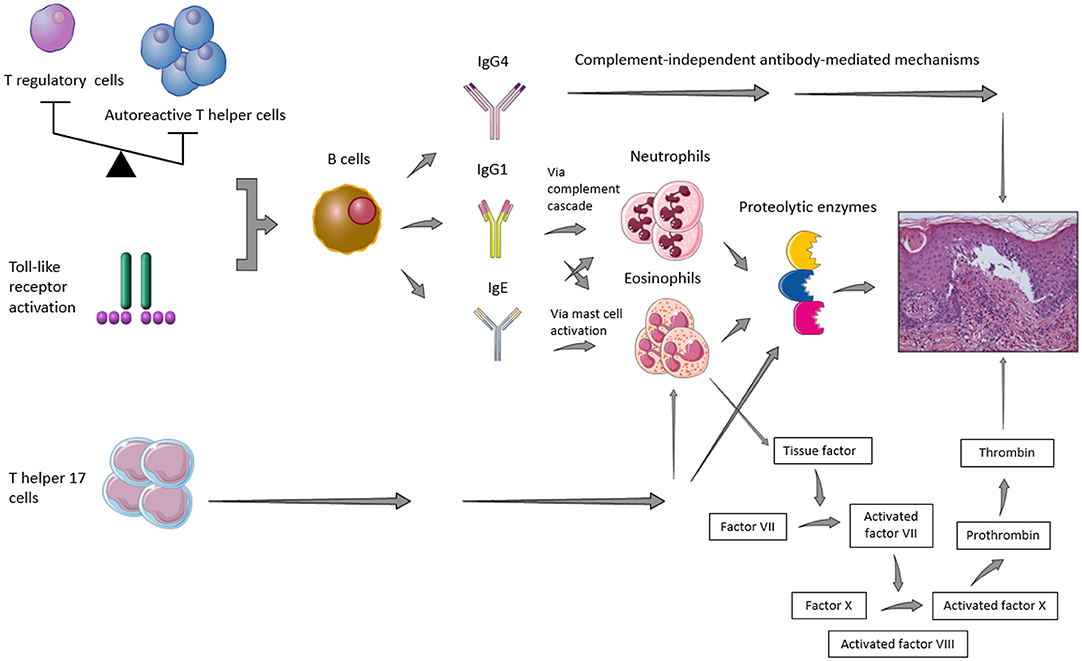
Autoimmune disorders occur when the body’s immune system, which normally protects against infections and diseases, begins attacking healthy cells and tissues. In the case of bullous pemphigoid, the immune system targets proteins that hold the layers of the skin together. This leads to the separation of these layers and the subsequent formation of blisters.
Causes of Bullous Pemphigoid
The exact cause of bullous pemphigoid remains unknown, but researchers believe it involves a combination of genetic and environmental factors. Below are some potential triggers and contributing factors:
Immune System Malfunction
In bullous pemphigoid, the immune system produces antibodies that attack specific proteins in the skin. These proteins, known as BP antigen one and BP antigen two, are essential for maintaining the structural integrity of the skin. When these proteins are targeted, the layers of the skin separate, leading to blister formation.
Genetic Predisposition
Some individuals may have a genetic predisposition to developing autoimmune conditions, including bullous pemphigoid. Certain genetic markers have been associated with an increased risk of this condition, suggesting that heredity may play a role.
Environmental Triggers
- Medications: Some medications, such as diuretics, antibiotics, and nonsteroidal anti-inflammatory drugs, have been linked to the onset of bullous pemphigoid in certain individuals.
- Infections: Viral or bacterial infections may act as triggers for the condition in susceptible individuals.
- Physical Trauma: Skin injuries, burns, or surgeries may sometimes precede the development of bullous pemphigoid.
Symptoms of Bullous Pemphigoid
The symptoms of bullous pemphigoid can vary from person to person, but they generally include the following:
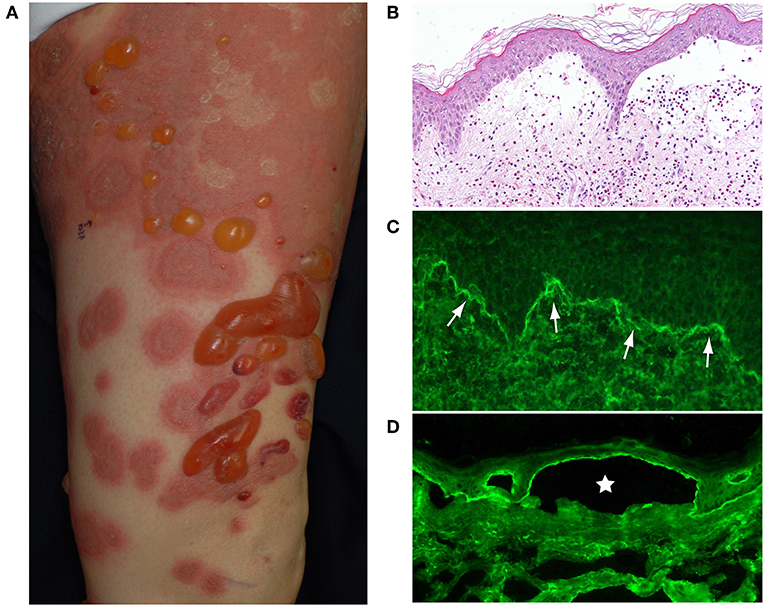
Skin Blisters
The hallmark symptom of bullous pemphigoid is the appearance of large, raised blisters on the skin. These blisters are typically filled with clear fluid and may appear on areas such as the arms, legs, abdomen, or groin. They are often described as tense and do not rupture easily.
Itching and Redness
Before the blisters form, many individuals experience intense itching and redness in the affected areas. This itching can be severe and may interfere with daily activities and sleep.
Eczema-like Rash
In some cases, individuals may develop a rash that resembles eczema before the blisters appear. This rash is often red, inflamed, and itchy.
Mouth Blisters
Although less common, bullous pemphigoid can also affect the mucous membranes, such as those inside the mouth. This can lead to the formation of painful blisters or sores in these areas.
Diagnosis of Bullous Pemphigoid
Diagnosing bullous pemphigoid can be challenging because its symptoms resemble those of other blistering skin conditions. A thorough evaluation by a healthcare professional is necessary to confirm the diagnosis. Below are the common diagnostic methods used:
Clinical Examination
A dermatologist will begin by examining the skin and assessing the appearance of the blisters. They may ask about the patient’s medical history, including any medications being taken or recent illnesses.
Skin Biopsy
A small sample of the affected skin may be removed and examined under a microscope. This procedure helps identify characteristic changes in the skin layers caused by bullous pemphigoid.
Direct Immunofluorescence Test
This test involves taking a biopsy of the skin and using special dyes to detect the presence of antibodies targeting the skin proteins. A positive result confirms the diagnosis of bullous pemphigoid.
Blood Tests
Blood tests may be conducted to check for the presence of specific antibodies associated with bullous pemphigoid. Elevated levels of these antibodies can support the diagnosis.
Treatment Options for Bullous Pemphigoid
While there is no cure for bullous pemphigoid, several treatment options are available to manage symptoms and prevent complications. The choice of treatment depends on the severity of the condition and the patient’s overall health. Below are the most common approaches:
Corticosteroids
Corticosteroids, such as prednisone, are often the first line of treatment for bullous pemphigoid. These medications work by suppressing the immune system and reducing inflammation. While effective, long-term use of corticosteroids can lead to side effects, so the dosage is usually tapered over time.
Immunosuppressive Medications
In cases where corticosteroids alone are insufficient, immunosuppressive drugs like azathioprine or mycophenolate mofetil may be prescribed. These medications help reduce the activity of the immune system and minimize blister formation.
Topical Treatments
For mild cases of bullous pemphigoid, topical corticosteroid creams or ointments may be applied directly to the affected areas. This approach helps reduce inflammation and promote healing without the systemic side effects of oral medications.
Antibiotics
In some cases, antibiotics such as tetracycline or dapsone may be used to treat bullous pemphigoid. These medications have anti-inflammatory properties and can help control the condition in certain individuals.
Wound Care
Proper wound care is essential to prevent infection and promote healing of the blisters. This may involve keeping the affected areas clean, applying dressings, and avoiding activities that could irritate the skin.
Lifestyle Modifications
Making certain lifestyle changes can also help manage bullous pemphigoid. These include:
- Avoiding scratching or rubbing the blisters to prevent further irritation.
- Using gentle skincare products that do not contain harsh chemicals or fragrances.
- Wearing loose-fitting clothing to reduce friction on the skin.
Potential Complications of Bullous Pemphigoid
If left untreated, bullous pemphigoid can lead to several complications, including:
- Infections: Open blisters can become infected, leading to additional health issues.
- Scarring: Severe blistering may result in permanent scarring or changes in skin pigmentation.
- Side Effects of Medications: Long-term use of corticosteroids or immunosuppressive drugs can cause significant side effects, such as osteoporosis, diabetes, or increased susceptibility to infections.
Living with Bullous Pemphigoid
Managing bullous pemphigoid requires ongoing care and attention. Regular follow-ups with a dermatologist are crucial to monitor the condition and adjust treatment as needed. Additionally, patients should be vigilant about identifying and avoiding potential triggers that could worsen their symptoms.
Support groups and counseling can also be beneficial for individuals dealing with bullous pemphigoid. Connecting with others who have the condition can provide emotional support and practical advice for coping with its challenges.
Research and Future Directions
Ongoing research is focused on better understanding the underlying mechanisms of bullous pemphigoid and developing more targeted treatments. Advances in immunology and genetics hold promise for improving outcomes for individuals with this condition. Clinical trials are exploring new therapies that may offer relief with fewer side effects than current options.
By staying informed and working closely with healthcare providers, individuals with bullous pemphigoid can achieve better control over their symptoms and improve their quality of life.