Brugada Syndrome, often abbreviated as BS, is a rare but potentially life-threatening heart condition that affects the way electrical signals travel through the heart. This disorder can lead to abnormal heart rhythms, known as arrhythmias, which may result in sudden cardiac arrest or death. While Brugada Syndrome is not widely known, it has gained attention in recent years due to its association with unexplained deaths in otherwise healthy individuals. In this article, we will explore what Brugada Syndrome is, how it affects the heart, its symptoms, diagnosis, treatment options, and ongoing research into this complex condition.
Understanding the Basics of Heart Rhythm Disorders
To comprehend Brugada Syndrome, it is essential to first understand how the heart functions under normal circumstances. The heart is an intricate organ that relies on electrical impulses to maintain a steady rhythm. These impulses originate in the sinoatrial node, often referred to as the natural pacemaker of the heart, and travel through specific pathways to coordinate the contraction of the heart’s chambers. When these electrical signals are disrupted, it can lead to various types of heart rhythm disorders.
Heart rhythm disorders, also known as arrhythmias, occur when the electrical activity of the heart is irregular or too fast or too slow. Some arrhythmias are harmless, while others can be dangerous or even fatal. Brugada Syndrome falls into the latter category because it predisposes individuals to ventricular fibrillation, a chaotic and rapid heart rhythm that prevents the heart from pumping blood effectively.
The Role of Genetics in Brugada Syndrome
One of the defining characteristics of Brugada Syndrome is its genetic basis. It is typically inherited in an autosomal dominant pattern, meaning that a person only needs to inherit one copy of the mutated gene from one parent to develop the condition. Several genes have been linked to Brugada Syndrome, with the most common being SCN5A. This gene provides instructions for making a protein that forms sodium channels in the heart, which are crucial for conducting electrical signals.
- Mutations in the SCN5A gene can disrupt the flow of sodium ions in heart cells, leading to abnormal electrical activity.
- Other genes, such as CACNA1C and GPD1L, have also been associated with the syndrome, highlighting its genetic complexity.
- Not everyone with a genetic mutation will develop symptoms, suggesting that environmental factors and other genetic modifiers may play a role.
Symptoms of Brugada Syndrome
One of the challenges of diagnosing Brugada Syndrome is that many individuals with the condition do not experience noticeable symptoms. However, when symptoms do occur, they can be severe and life-threatening. The most common symptoms include:
- Fainting spells, also known as syncope, which occur due to a sudden drop in blood pressure caused by an irregular heartbeat.
- Seizure-like episodes, which may be mistaken for epilepsy if the underlying heart condition is not identified.
- Sudden cardiac arrest, where the heart stops beating entirely, often without warning.
In some cases, symptoms may appear during sleep, making them difficult to detect. This has led researchers to speculate that Brugada Syndrome may be responsible for some cases of sudden unexpected nocturnal death syndrome, particularly in Southeast Asian populations.
Triggers for Symptoms
Certain factors can trigger symptoms in individuals with Brugada Syndrome. These triggers include:
- High body temperature, such as during a fever, which can exacerbate electrical instability in the heart.
- Certain medications, including those used to treat depression, high blood pressure, and other conditions, which may interfere with the heart’s electrical system.
- Excessive alcohol consumption, which can strain the heart and increase the risk of arrhythmias.
Diagnosing Brugada Syndrome
Diagnosing Brugada Syndrome can be challenging because its symptoms are often nonspecific and may mimic other conditions. A thorough evaluation is required to confirm the presence of the disorder. The diagnostic process typically involves the following steps:
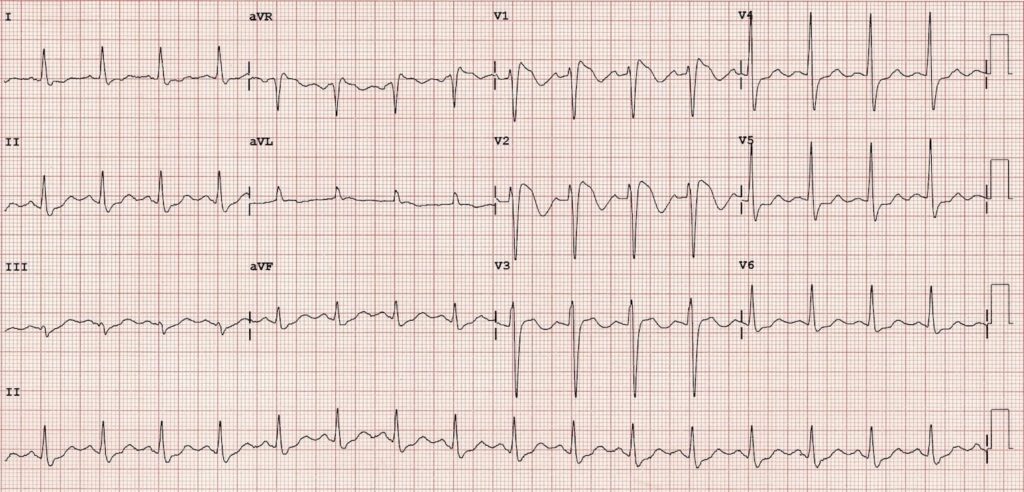
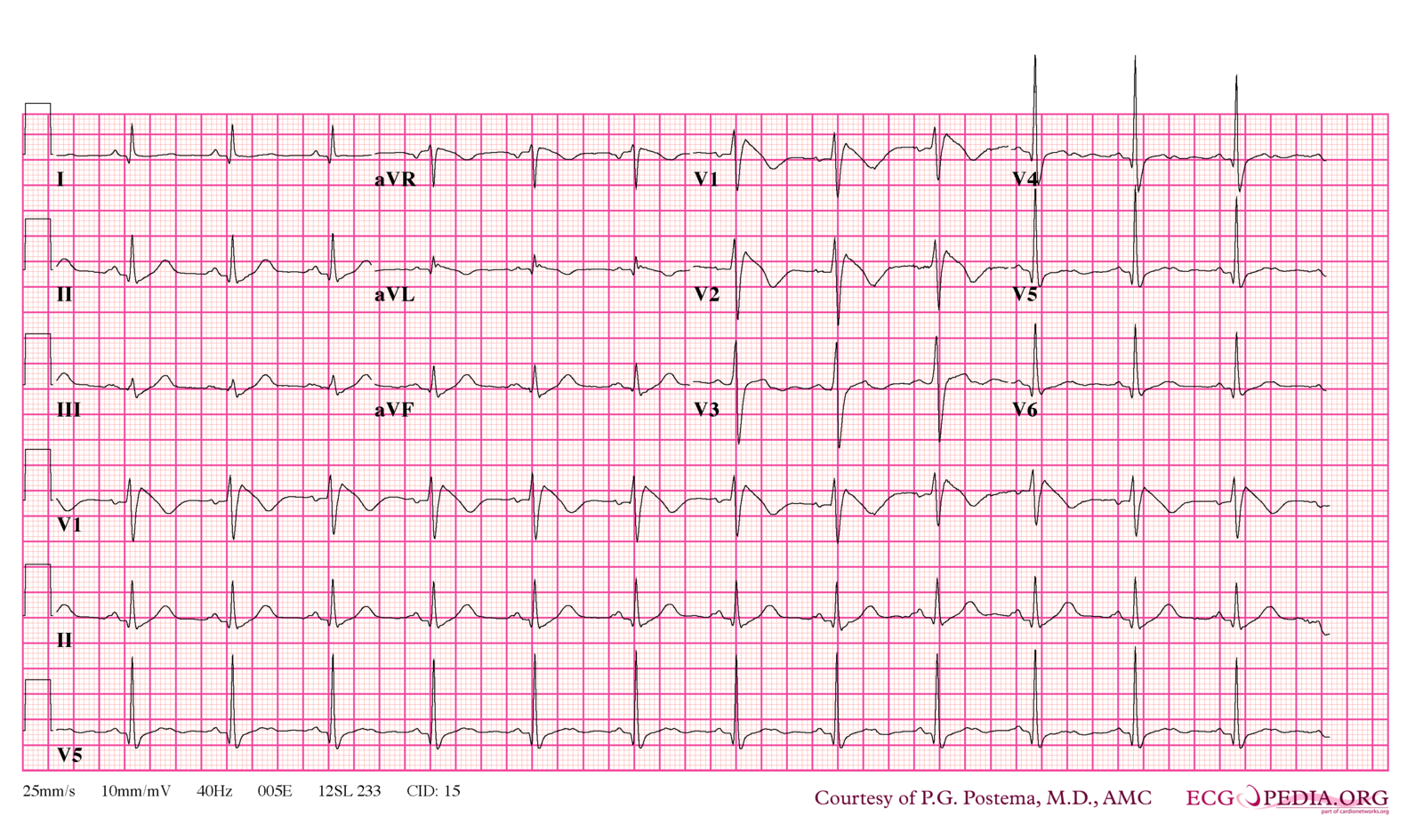
Electrocardiogram (ECG)
An electrocardiogram is the primary tool used to diagnose Brugada Syndrome. This noninvasive test records the electrical activity of the heart and can reveal characteristic patterns associated with the condition. In particular, doctors look for a specific pattern known as a “coved-type” ST-segment elevation in leads V1 and V2 of the ECG. This pattern indicates abnormal electrical activity in the right ventricle of the heart.
In some cases, the ECG may not show clear signs of Brugada Syndrome at first. To uncover hidden abnormalities, a doctor may perform a drug challenge test using medications like ajmaline or flecainide. These drugs temporarily block sodium channels in the heart, making it easier to detect underlying electrical issues.
Genetic Testing
Genetic testing is another important component of diagnosing Brugada Syndrome. By analyzing a patient’s DNA, doctors can identify mutations in genes associated with the condition. While a positive genetic test can confirm the diagnosis, a negative result does not rule out Brugada Syndrome, as not all cases are linked to known genetic mutations.
Family History Assessment
Because Brugada Syndrome is often inherited, assessing a patient’s family history is critical. Doctors will inquire about any instances of sudden cardiac death, unexplained fainting, or seizures in close relatives. If a family member has been diagnosed with Brugada Syndrome, it increases the likelihood that other family members may also be affected.
Treatment Options for Brugada Syndrome
Currently, there is no cure for Brugada Syndrome. However, several treatment strategies are available to manage the condition and reduce the risk of complications. The choice of treatment depends on the severity of the condition and whether the individual has experienced symptoms.
Implantable Cardioverter-Defibrillator (ICD)
For individuals who have experienced symptoms such as fainting or cardiac arrest, an implantable cardioverter-defibrillator is often recommended. This small device is surgically placed under the skin and continuously monitors the heart’s rhythm. If it detects a dangerous arrhythmia, the ICD delivers an electric shock to restore a normal heartbeat.
While ICDs are highly effective at preventing sudden cardiac death, they are not without risks. Potential complications include infection, device malfunction, and inappropriate shocks, which can be distressing for patients.
Medications
Quinidine, an antiarrhythmic medication, is sometimes prescribed to individuals with Brugada Syndrome. This drug works by stabilizing the heart’s electrical activity and reducing the risk of arrhythmias. However, quinidine is not suitable for everyone and may cause side effects such as gastrointestinal upset and low blood pressure.
It is important for patients to avoid medications that can exacerbate their condition. A comprehensive list of drugs to avoid is available through resources like the Brugada Drugs to Avoid List, which is regularly updated by medical professionals.
Lifestyle Modifications
In addition to medical interventions, lifestyle changes can help manage Brugada Syndrome. These include:
- Avoiding excessive alcohol consumption, which can trigger arrhythmias.
- Staying hydrated and managing fevers promptly to prevent overheating.
- Engaging in regular, moderate exercise, while avoiding extreme physical exertion that could strain the heart.
Ongoing Research and Future Directions
Despite advances in understanding Brugada Syndrome, many questions remain unanswered. Researchers are actively investigating new ways to improve diagnosis, treatment, and prevention of the condition. Some areas of focus include:
Advanced Genetic Studies
Scientists are working to identify additional genes and molecular pathways involved in Brugada Syndrome. By gaining a deeper understanding of the genetic underpinnings of the disorder, researchers hope to develop targeted therapies that address the root cause of the condition.
Novel Therapies
Experimental treatments, such as gene therapy and stem cell therapy, hold promise for repairing damaged heart tissue and restoring normal electrical function. While these approaches are still in the early stages of development, they represent exciting possibilities for the future.
Improved Risk Stratification
Another key area of research is improving methods for predicting which individuals with Brugada Syndrome are at the highest risk of experiencing life-threatening arrhythmias. By refining risk assessment tools, doctors can tailor treatment plans to each patient’s unique needs.
Raising Awareness About Brugada Syndrome
Because Brugada Syndrome is relatively rare and often asymptomatic, raising awareness is crucial for early detection and prevention. Public education campaigns, support groups, and advocacy organizations play an important role in spreading information about the condition. Healthcare providers also have a responsibility to educate patients and their families about the potential risks and warning signs.
By fostering greater understanding of Brugada Syndrome, we can empower individuals to seek timely medical care and take proactive steps to protect their heart health.