Brucellosis, also known as Undulant Fever, is a bacterial infection that primarily affects animals but can be transmitted to humans. The condition is caused by bacteria of the genus Brucella and poses significant health risks if left untreated. This article explores the causes, symptoms, diagnosis, and treatment options for this infectious disease.
What is Brucellosis?
Brucellosis is an infectious disease that spreads from animals to humans. It is characterized by symptoms such as fever, fatigue, and joint pain. The disease is most commonly found in regions where livestock is raised, and it has been reported worldwide, particularly in areas with limited access to healthcare and proper animal management practices.
History of Brucellosis
The disease was first identified in the 19th century when it was observed in people who consumed raw milk or came into close contact with infected animals. Over time, scientists discovered that the bacteria responsible for the disease could survive in various environments, making it challenging to eradicate completely.
Causes of Brucellosis
Brucellosis is caused by bacteria belonging to the genus Brucella. These bacteria are highly contagious and can infect both animals and humans. Understanding the sources of infection and how the bacteria spread is crucial for prevention and control.
Primary Sources of Infection
- Infected Animals: The bacteria are commonly found in domesticated animals such as cattle, goats, sheep, and pigs. Humans can contract the disease through direct contact with infected animals or their bodily fluids.
- Contaminated Food: Consuming unpasteurized milk or dairy products made from infected animals is a common cause of brucellosis in humans.
- Inhalation: In rare cases, the bacteria can be inhaled, especially in laboratory settings or areas where animal products are processed.
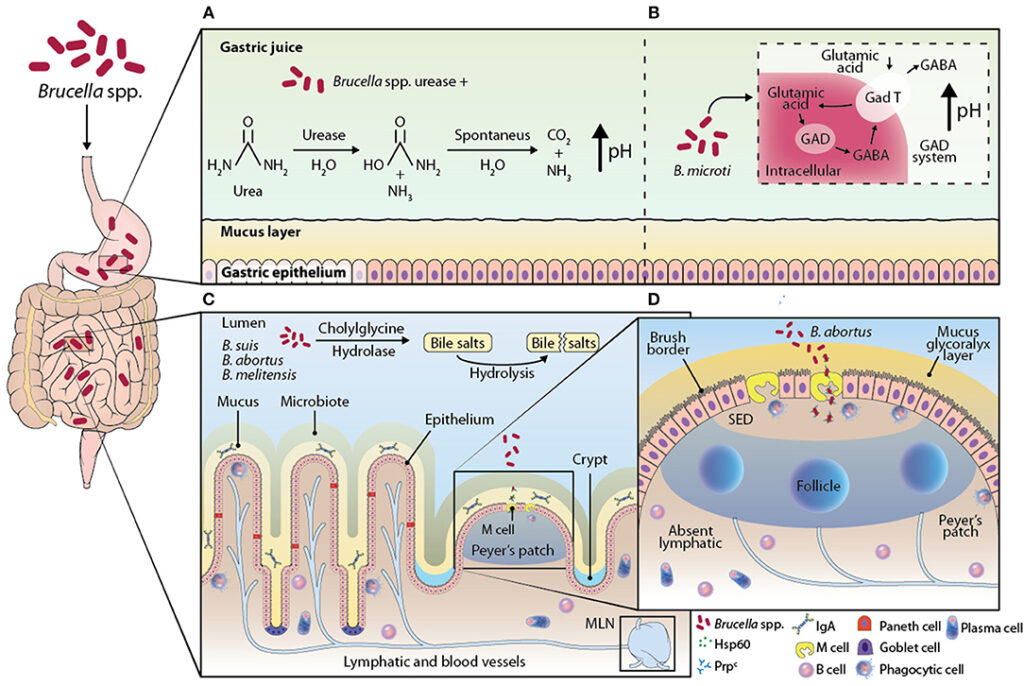
How Brucella Bacteria Spread
The bacteria enter the human body through breaks in the skin, inhalation, or ingestion. Once inside, they invade the bloodstream and lymphatic system, causing systemic infections. The bacteria can survive and multiply within host cells, leading to prolonged illness if not treated promptly.
Symptoms of Brucellosis
The symptoms of brucellosis can vary depending on the severity of the infection and the individual’s immune response. Some people may experience mild symptoms, while others may develop severe complications.
Common Symptoms
- Fever: One of the hallmark symptoms of brucellosis is intermittent fever, which often rises and falls over weeks or months.
- Fatigue: Patients frequently report extreme tiredness and weakness, which can interfere with daily activities.
- Muscle and Joint Pain: Pain in the muscles and joints is common, often resembling symptoms of arthritis.
- Night Sweats: Profuse sweating during the night is another characteristic symptom of the disease.
- Headaches: Many individuals experience persistent headaches, which can range from mild to severe.
Less Common Symptoms
- Swollen Lymph Nodes: Enlarged lymph nodes may occur in some cases, indicating an active immune response.
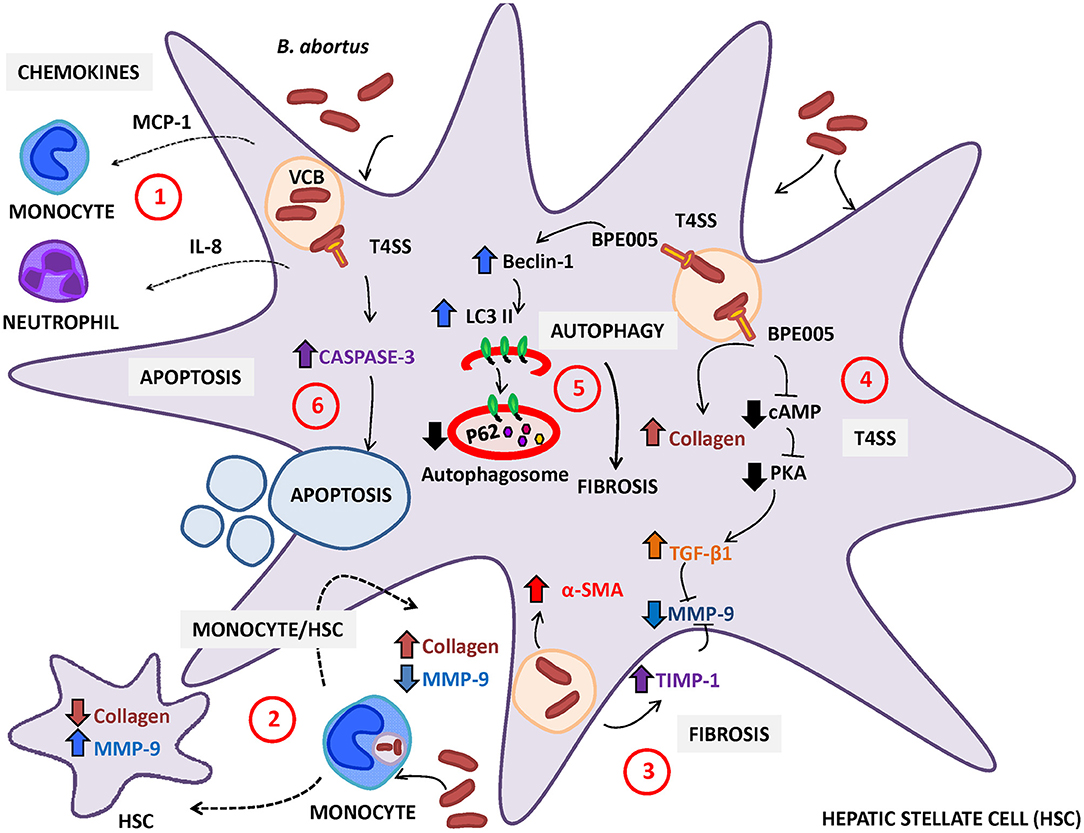
- Liver or Spleen Enlargement: In severe cases, the liver or spleen may become enlarged, leading to abdominal discomfort.
- Neurological Issues: Rarely, the infection can affect the central nervous system, causing symptoms such as confusion or seizures.
Diagnosis of Brucellosis
Diagnosing brucellosis can be challenging because its symptoms resemble those of other diseases. A combination of clinical evaluation, laboratory tests, and patient history is essential for accurate diagnosis.
Clinical Evaluation
Healthcare providers begin by assessing the patient’s medical history, including recent exposure to animals or consumption of unpasteurized dairy products. They also perform a physical examination to check for signs such as fever, swollen lymph nodes, or joint pain.
Laboratory Tests
- Blood Tests: Blood samples are analyzed to detect antibodies against the bacteria. Elevated levels of specific antibodies indicate an active infection.
- Culture Tests: Growing the bacteria from blood, bone marrow, or other bodily fluids in a laboratory setting confirms the presence of the bacteria.
- Imaging Studies: In cases where complications are suspected, imaging techniques like X-rays or ultrasounds may be used to examine affected organs.
Differential Diagnosis
Since brucellosis shares symptoms with other conditions such as tuberculosis, malaria, and typhoid fever, ruling out these diseases is critical. Healthcare providers may order additional tests to ensure an accurate diagnosis.
Treatment Options for Brucellosis
While brucellosis can be debilitating, it is treatable with appropriate medical intervention. Early diagnosis and treatment are key to preventing complications and ensuring a full recovery.
Antibiotic Therapy
The primary treatment for brucellosis involves a course of antibiotics. The choice of antibiotics depends on the severity of the infection and the patient’s overall health.
- Doxycycline and Rifampin: This combination is commonly prescribed for at least six weeks to effectively eliminate the bacteria.
- Streptomycin: In more severe cases, streptomycin may be added to the treatment regimen for a short period to enhance effectiveness.
- Alternative Medications: For patients who cannot tolerate standard antibiotics, alternative medications such as trimethoprim-sulfamethoxazole may be considered.
Supportive Care
In addition to antibiotics, supportive care measures are often recommended to manage symptoms and improve the patient’s quality of life.
- Pain Management: Over-the-counter pain relievers can help alleviate muscle and joint pain.
- Rest and Hydration: Adequate rest and hydration are essential for recovery, especially during periods of high fever.
- Nutritional Support: A balanced diet rich in vitamins and minerals supports the immune system and aids in healing.
Monitoring and Follow-Up
Patients undergoing treatment for brucellosis require regular monitoring to assess their progress and ensure the infection is fully eradicated. Follow-up appointments may include repeat blood tests and evaluations for potential complications.
Prevention of Brucellosis
Preventing brucellosis involves reducing exposure to the bacteria and implementing effective public health measures. Both individuals and communities play a role in minimizing the risk of infection.
Personal Prevention Strategies
- Avoid Unpasteurized Dairy Products: Consuming only pasteurized milk and cheese significantly reduces the risk of infection.
- Practice Good Hygiene: Washing hands thoroughly after handling animals or animal products is crucial for prevention.
- Use Protective Gear: Individuals working in veterinary or agricultural settings should wear gloves and masks to minimize exposure.
Public Health Measures
- Vaccination of Livestock: Vaccinating animals against brucellosis helps reduce the prevalence of the disease in livestock populations.
- Surveillance Programs: Monitoring and reporting cases of brucellosis in animals and humans enable early detection and intervention.
- Educational Campaigns: Raising awareness about the disease and its transmission routes empowers communities to take preventive actions.
Complications of Untreated Brucellosis
If left untreated, brucellosis can lead to serious complications that affect multiple organ systems. Timely treatment is essential to avoid long-term health consequences.
Chronic Fatigue Syndrome
Many patients with untreated brucellosis develop chronic fatigue syndrome, characterized by persistent exhaustion that does not improve with rest.
Joint Damage
Long-term inflammation of the joints can result in permanent damage, leading to reduced mobility and chronic pain.
Endocarditis
In rare cases, the bacteria can infect the heart valves, causing endocarditis, a potentially life-threatening condition.
Neurological Complications
Brucellosis can affect the nervous system, leading to conditions such as meningitis or encephalitis, which require immediate medical attention.