Bone infection, also known as osteomyelitis, is a serious medical condition that requires prompt attention. Osteomyelitis can affect individuals of all ages and may lead to severe complications if not treated effectively. This article delves into the causes, symptoms, diagnosis methods, and treatment options available for managing this condition.
Understanding Bone Infection
Bone infection occurs when bacteria or other microorganisms invade the bone tissue, leading to inflammation and damage. The infection can either be acute, developing suddenly, or chronic, persisting over a long period. While bones are typically resistant to infections due to their limited blood supply, certain factors can make them vulnerable to microbial invasion.
Causes of Bone Infection
The primary cause of bone infection is the spread of bacteria or fungi into the bone tissue. Several pathways can lead to this:
- Bloodstream Infection: Microorganisms from an infection elsewhere in the body can travel through the bloodstream and settle in the bones. This is more common in children, where growing bones have a richer blood supply.
- Injury or Trauma: Open fractures or deep wounds that expose the bone to external contaminants can introduce bacteria directly into the bone tissue.
- Surgical Procedures: Surgeries involving bones, such as joint replacements or fracture repairs, carry a risk of introducing infections if proper sterilization protocols are not followed.
- Weakened Immune System: Individuals with compromised immune systems, such as those with diabetes, HIV/AIDS, or undergoing chemotherapy, are at higher risk of developing bone infections.
Symptoms of Bone Infection
The symptoms of bone infection vary depending on the severity and location of the infection. Common signs include:
- Pain and tenderness in the affected area
- Swelling, redness, or warmth around the infected bone
- Fever and chills
- Drainage of pus through the skin if the infection breaks through the surface
- Restricted movement in nearby joints
- General fatigue and malaise
In chronic cases, symptoms may develop gradually and be less pronounced, making diagnosis more challenging.
Diagnosing Bone Infection
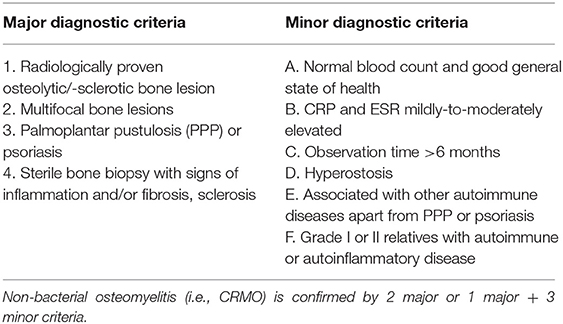
Accurate diagnosis is crucial for effective treatment of bone infections. Healthcare providers use a combination of clinical evaluation, imaging tests, and laboratory analyses to confirm the presence of an infection.
Clinical Evaluation
A thorough physical examination and review of the patient’s medical history are the first steps in diagnosing bone infection. The healthcare provider will assess symptoms, inquire about recent injuries or surgeries, and evaluate risk factors such as underlying health conditions.
Imaging Tests
Several imaging techniques are employed to visualize the bone and surrounding tissues:
- X-rays: X-rays can reveal bone damage, but they may not detect early-stage infections.
- Magnetic Resonance Imaging (MRI): MRI provides detailed images of soft tissues and bones, making it highly effective for identifying infections.
- Computed Tomography (CT) Scan: CT scans offer cross-sectional views of the bone and can help identify abscesses or areas of dead tissue.
- Bone Scans: A radioactive tracer is injected into the bloodstream, and its accumulation in the bone helps pinpoint infection sites.
Laboratory Tests
Blood tests and cultures play a critical role in confirming the diagnosis:
- Blood Tests: Elevated white blood cell counts and markers of inflammation, such as C-reactive protein, indicate an ongoing infection.
- Bone Biopsy: A small sample of bone tissue is extracted and analyzed to identify the specific microorganism causing the infection. This helps guide antibiotic therapy.
- Culture of Drainage: If there is pus or fluid discharge, it is cultured to determine the causative agent.
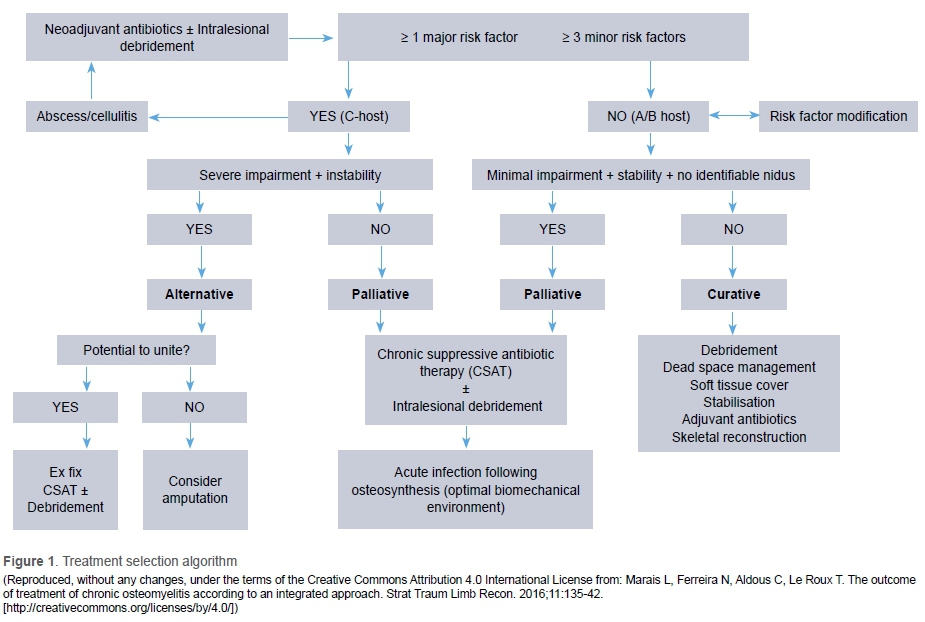
Treatment Options for Bone Infection
Treating bone infection often requires a multidisciplinary approach, combining medications, surgical interventions, and supportive therapies. The goal is to eliminate the infection, preserve bone function, and prevent recurrence.
Antibiotic Therapy
Antibiotics are the cornerstone of treatment for bone infections. The choice of antibiotic depends on the type of microorganism identified during diagnosis. Treatment typically involves:
- Intravenous Antibiotics: For severe infections, antibiotics are administered intravenously in a hospital setting for several weeks.
- Oral Antibiotics: Once the infection is under control, patients may transition to oral antibiotics for an extended period.
- Long-Term Therapy: Chronic infections may require months of antibiotic treatment to ensure complete eradication of the bacteria.
Surgical Interventions
In cases where antibiotics alone are insufficient, surgery may be necessary to remove infected tissue and restore bone integrity:
- Debridement: Infected and dead bone tissue is surgically removed to prevent the spread of infection.
- Drainage of Abscesses: Pus-filled pockets are drained to relieve pressure and reduce bacterial load.
- Bone Grafts: Damaged bone segments may be replaced with healthy bone tissue from another part of the body or a donor.
- Stabilization of Fractures: If the infection has weakened the bone, surgical stabilization using plates, screws, or rods may be required.
Supportive Therapies
Additional measures can aid recovery and improve outcomes:
- Pain Management: Pain relievers and anti-inflammatory medications help alleviate discomfort during treatment.
- Wound Care: Proper cleaning and dressing of open wounds prevent secondary infections.
- Nutritional Support: A balanced diet rich in vitamins and minerals promotes healing and strengthens the immune system.
- Physical Therapy: Rehabilitation exercises restore mobility and function to affected joints and muscles.
Preventing Bone Infections
While not all cases of bone infection can be prevented, certain measures can reduce the risk:
- Seek prompt treatment for infections, especially those near the bones or joints.
- Follow strict hygiene practices during wound care and after surgeries.
- Manage underlying health conditions, such as diabetes, to minimize susceptibility to infections.
- Vaccinate against common pathogens, such as Staphylococcus aureus, if recommended by a healthcare provider.
Challenges in Managing Bone Infections
Despite advances in medical science, treating bone infections remains challenging due to several factors:
- Delayed Diagnosis: Early symptoms may be subtle, leading to delayed recognition and treatment.
- Antibiotic Resistance: Some bacteria have developed resistance to commonly used antibiotics, complicating treatment.
- Chronic Nature: Recurrent or persistent infections require long-term management and frequent monitoring.
- Impact on Quality of Life: Prolonged treatment and potential disability can significantly affect a patient’s well-being.
Addressing these challenges requires ongoing research, improved diagnostic tools, and innovative treatment strategies.