Body Dysmorphic Disorder, commonly referred to as BDD, is a mental health condition characterized by obsessive focus on perceived flaws in physical appearance. Individuals with this condition often experience significant distress and may go to great lengths to hide or fix their perceived imperfections. While many people have moments of dissatisfaction with their appearance, those with Body Dysmorphic Disorder experience these feelings intensely and persistently, impacting their daily lives and overall well-being. This article delves into the symptoms, causes, and treatments associated with this challenging disorder.
Understanding the Symptoms
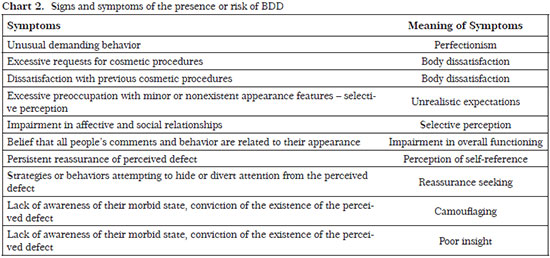
The symptoms of Body Dysmorphic Disorder can vary from person to person, but they generally revolve around an intense preoccupation with one’s appearance. These symptoms are not just about vanity; they are deeply rooted in anxiety and emotional distress. Below are some common signs that someone might be struggling with this condition:
Obsessive Focus on Appearance
- Constantly checking mirrors or avoiding them altogether
- Frequent comparison of one’s appearance to others
- Excessive grooming, such as combing hair repeatedly or applying makeup excessively
Individuals with this condition may spend hours each day focusing on their perceived flaws, which can include anything from skin texture and facial features to body shape and size. This obsession can interfere with work, school, and social interactions.
Emotional Distress and Avoidance
- Avoiding social situations due to fear of judgment
- Feeling anxious or depressed because of perceived flaws
- Seeking reassurance from others about appearance but never feeling satisfied
People with this disorder often feel overwhelmed by shame and embarrassment, leading them to isolate themselves from friends and family. They may also avoid activities they once enjoyed, such as going to the beach or attending social gatherings, out of fear that others will notice their flaws.
Compulsive Behaviors
- Frequent visits to dermatologists or plastic surgeons for procedures
- Engaging in repetitive behaviors like picking at skin or excessive exercising
- Wearing excessive makeup or clothing to conceal perceived imperfections
These compulsive behaviors are attempts to alleviate the distress caused by the perceived flaws. However, they often provide only temporary relief and can exacerbate the problem over time.
Exploring the Causes
The exact cause of Body Dysmorphic Disorder is not fully understood, but research suggests that it arises from a combination of biological, psychological, and environmental factors. Understanding these potential causes can help shed light on why some individuals develop this condition while others do not.
Biological Factors
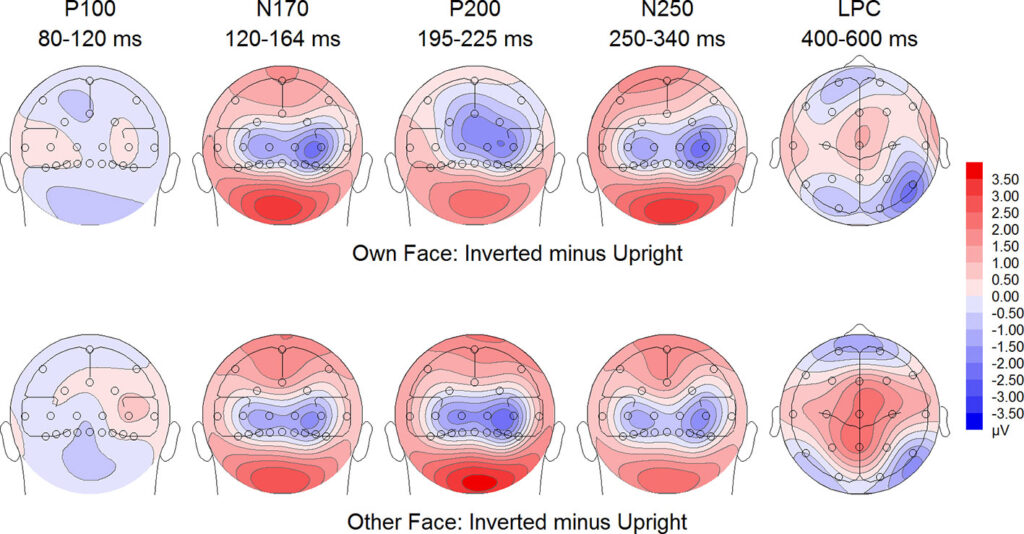
There is evidence to suggest that genetics may play a role in the development of this condition. Studies have shown that individuals with a family history of obsessive-compulsive disorder or other related conditions may be more susceptible to developing similar issues. Additionally, abnormalities in brain structure or function, particularly in areas related to processing visual information and regulating emotions, may contribute to the disorder.
Psychological Factors
Low self-esteem and perfectionism are common traits among individuals with this condition. Many people who struggle with this disorder have a distorted self-image and set unrealistically high standards for their appearance. Childhood experiences, such as bullying or teasing about one’s looks, can also leave lasting emotional scars that manifest later in life as obsessive thoughts about appearance.
Environmental Influences
Societal pressures and media portrayals of beauty can significantly impact how individuals perceive themselves. Constant exposure to images of “ideal” bodies and faces can create unrealistic expectations and fuel dissatisfaction with one’s own appearance. Peer pressure and cultural norms regarding attractiveness may further exacerbate these feelings, especially during adolescence when identity formation is crucial.
Treatment Options
While there is no cure for Body Dysmorphic Disorder, several treatment options can help manage symptoms and improve quality of life. A combination of therapy, medication, and lifestyle changes is often recommended for the best outcomes.
Cognitive Behavioral Therapy
Cognitive behavioral therapy is considered one of the most effective treatments for this condition. This form of therapy focuses on identifying and challenging negative thought patterns related to appearance. Through guided sessions with a trained therapist, individuals learn to reframe their perceptions and develop healthier coping mechanisms. Exposure therapy, a component of cognitive behavioral therapy, involves gradually confronting feared situations without resorting to compulsive behaviors, helping reduce anxiety over time.
Medication
In some cases, medication may be prescribed to help manage symptoms. Selective serotonin reuptake inhibitors, commonly used to treat depression and anxiety, have shown promise in alleviating obsessive thoughts and compulsive behaviors associated with this condition. It is important to note that medication should always be taken under the guidance of a qualified healthcare professional and is most effective when combined with therapy.
Support Groups
Joining support groups can provide individuals with a sense of community and understanding. Sharing experiences with others who face similar challenges can reduce feelings of isolation and offer practical advice for managing symptoms. Support groups may be available in-person or online, making them accessible to a wide range of individuals.
Lifestyle Changes
Making certain lifestyle adjustments can complement professional treatment. Regular exercise, a balanced diet, and adequate sleep can improve overall mental health and resilience. Mindfulness practices, such as meditation and yoga, can also help individuals become more aware of their thoughts and emotions, reducing the intensity of obsessive thinking.
Challenges in Diagnosis and Treatment
One of the biggest hurdles in addressing this condition is the stigma surrounding mental health. Many individuals may feel ashamed or embarrassed to seek help, fearing judgment from others. Additionally, the secretive nature of the disorder—such as hiding compulsive behaviors or downplaying symptoms—can make it difficult for loved ones and healthcare providers to recognize the problem.
Barriers to Seeking Help
- Fear of being labeled “vain” or “superficial”
- Lack of awareness about the condition among healthcare professionals
- Misdiagnosis due to overlapping symptoms with other disorders, such as obsessive-compulsive disorder or eating disorders
Education and open dialogue are essential to overcoming these barriers. By raising awareness about the seriousness of this condition, more individuals may feel empowered to seek the help they need.
The Role of Family and Friends
Support from loved ones can play a critical role in recovery. Family members and friends can encourage individuals to seek professional help and provide emotional support throughout the treatment process. However, it is important for supporters to approach the situation with empathy and understanding, avoiding dismissive comments like “you look fine” or “it’s all in your head,” which can invalidate the individual’s experience.
Living with Body Dysmorphic Disorder
Managing this condition requires ongoing effort and commitment. While setbacks are common, progress is possible with the right tools and support system. Individuals are encouraged to celebrate small victories, such as resisting the urge to check their appearance in the mirror or attending a social event despite anxiety.
Building Resilience
Developing resilience involves cultivating a positive mindset and learning to tolerate discomfort. Techniques such as journaling, practicing gratitude, and setting realistic goals can foster a sense of accomplishment and self-worth beyond physical appearance.
Advocacy and Awareness
Many individuals who have successfully managed their symptoms choose to become advocates for mental health awareness. By sharing their stories and educating others, they contribute to reducing stigma and encouraging early intervention for those struggling with similar issues.