An epidural hematoma, often abbreviated as EDH, is a serious medical condition that occurs when blood accumulates between the skull and the outermost protective layer of the brain. This type of bleeding can lead to increased pressure on the brain, causing potentially life-threatening complications if not promptly addressed. Understanding the causes, symptoms, diagnosis, and treatment options for this condition is crucial for both healthcare professionals and the general public. In this article, we will delve into the details of this condition, exploring its pathophysiology, risk factors, and management strategies.
What Is an Epidural Hematoma?
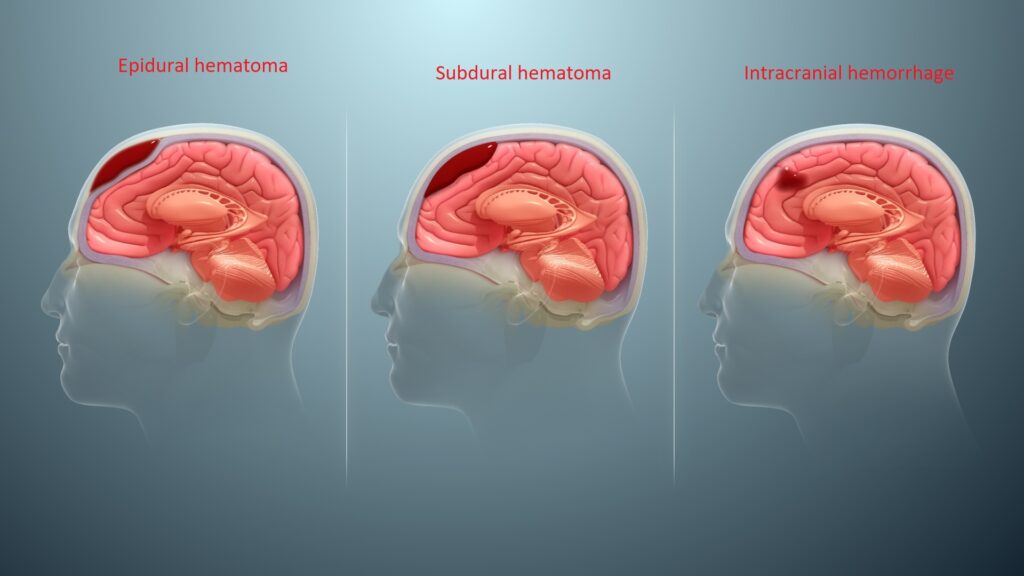
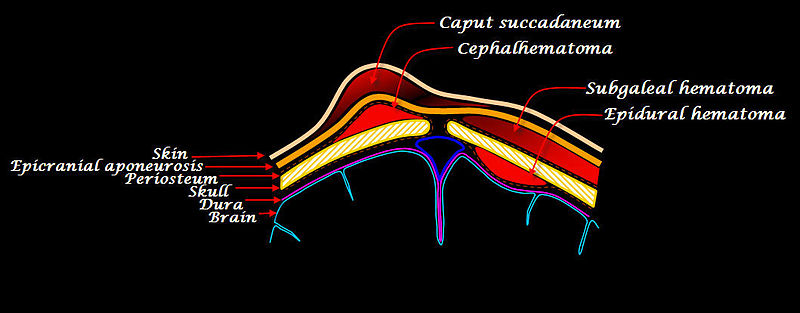
An epidural hematoma refers to the collection of blood between the dura mater, which is the tough outer membrane covering the brain, and the inner surface of the skull. The bleeding typically originates from a torn artery or vein, most commonly the middle meningeal artery, which runs close to the skull. When this artery is damaged, it can cause rapid accumulation of blood, leading to compression of the brain tissue beneath it.
This condition is often associated with traumatic head injuries, such as those sustained in car accidents, falls, or sports-related incidents. However, it can also occur in non-traumatic settings, although such cases are rare. The hallmark feature of an epidural hematoma is its potential to cause rapid neurological deterioration if left untreated.
How Does It Happen?
The development of an epidural hematoma usually follows a specific sequence of events:
- Trauma to the Head: A significant blow to the head can fracture the skull and damage blood vessels located near the surface of the brain.
- Bleeding Begins: Once a blood vessel is torn, blood starts to leak into the space between the skull and the dura mater.
- Accumulation of Blood: As the blood continues to collect, it forms a mass that exerts pressure on the brain.
- Increase in Intracranial Pressure: The growing hematoma compresses the brain tissue, disrupting normal brain function and potentially leading to severe complications.
Symptoms of an Epidural Hematoma
The symptoms of an epidural hematoma can vary depending on the size of the hematoma, the location of the bleeding, and the individual’s overall health. Some people may experience immediate and severe symptoms, while others might have a period of apparent recovery before symptoms worsen. Below are the common signs and symptoms associated with this condition:
- Headache: A sudden and intense headache is often one of the first symptoms experienced by individuals with an epidural hematoma.
- Nausea and Vomiting: These symptoms may occur due to increased intracranial pressure.
- Confusion or Altered Mental State: Patients may appear disoriented, have difficulty concentrating, or exhibit changes in behavior.
- Seizures: In some cases, seizures may occur as a result of the pressure exerted on the brain.
- Weakness or Paralysis: Depending on the location of the hematoma, individuals may experience weakness or loss of movement in certain parts of the body.
- Loss of Consciousness: This symptom can range from brief periods of unconsciousness to a deep coma.
It is important to note that some individuals may initially appear fine after a head injury, only to develop symptoms later. This phenomenon, known as the “lucid interval,” can be particularly dangerous because it may delay seeking medical attention.
When to Seek Medical Attention
If you or someone else experiences any of the following after a head injury, it is critical to seek emergency medical care immediately:
- A persistent or worsening headache
- Repeated vomiting
- Difficulty staying awake or alert
- Unequal pupil size
- Seizures
- Weakness or numbness in any part of the body
Diagnosing an Epidural Hematoma
Diagnosing an epidural hematoma requires a combination of clinical evaluation and imaging studies. Healthcare providers will begin by taking a detailed history of the injury and assessing the patient’s symptoms. They will also perform a thorough physical examination, paying close attention to neurological signs such as reflexes, coordination, and mental status.
Imaging Studies
To confirm the presence of an epidural hematoma, imaging tests are essential. The most commonly used diagnostic tools include:
- Computed Tomography (CT) Scan: A CT scan is the preferred imaging modality for detecting an epidural hematoma. It provides detailed images of the brain and can clearly show the location and size of the hematoma.
- Magnetic Resonance Imaging (MRI): While not as commonly used as a CT scan, an MRI may be ordered in certain cases to provide additional information about the extent of the injury.
In addition to imaging, laboratory tests such as blood work may be performed to assess the patient’s overall health and rule out other potential causes of their symptoms.
Treatment Options for an Epidural Hematoma
The treatment of an epidural hematoma depends on several factors, including the size of the hematoma, the severity of symptoms, and the patient’s overall condition. In general, there are two main approaches to managing this condition: conservative treatment and surgical intervention.
Conservative Treatment
For small hematomas that do not cause significant symptoms or increase in size, conservative treatment may be sufficient. This approach typically involves:
- Close Monitoring: Patients are closely observed in a hospital setting to ensure that their condition does not worsen.
- Pain Management: Medications may be prescribed to alleviate headaches and other discomforts.
- Preventing Further Injury: Measures are taken to protect the patient from additional trauma, such as restricting physical activity.
Surgical Intervention
In cases where the hematoma is large, causing significant symptoms, or leading to increased intracranial pressure, surgery is often required. The primary goal of surgery is to remove the accumulated blood and relieve pressure on the brain. Common surgical procedures include:
- Cranial Drilling: A small hole is drilled into the skull to drain the hematoma.
- Cranial Craniotomy: A larger section of the skull is removed to access and remove the hematoma.
Following surgery, patients are closely monitored in an intensive care unit to ensure proper recovery and to manage any complications that may arise.
Risk Factors for Developing an Epidural Hematoma
While anyone can develop an epidural hematoma, certain factors increase the likelihood of this condition occurring. These include:
- Age: Younger individuals, particularly children and adolescents, are at higher risk due to the elasticity of their skulls, which makes them more prone to fractures.
- Participation in High-Risk Activities: Engaging in contact sports, riding motorcycles without a helmet, or working in environments with a high risk of head injury increases the chances of sustaining a traumatic head injury.
- Alcohol and Drug Use: Intoxication impairs judgment and coordination, making individuals more susceptible to accidents and injuries.
- Underlying Medical Conditions: Conditions such as coagulopathy (bleeding disorders) or the use of blood-thinning medications can increase the risk of bleeding following a head injury.
Preventive Measures
While it may not always be possible to prevent an epidural hematoma, certain measures can reduce the risk of sustaining a head injury:
- Wear appropriate protective gear, such as helmets, during sports and recreational activities.
- Follow traffic safety rules and avoid driving under the influence of alcohol or drugs.
- Ensure that living spaces are free of tripping hazards to minimize the risk of falls.
- Seek medical advice before participating in activities that carry a high risk of head injury.
Complications Associated with an Epidural Hematoma
If left untreated, an epidural hematoma can lead to serious and potentially fatal complications. These include:
- Brain Herniation: Increased pressure on the brain can force brain tissue to shift, leading to herniation and permanent damage.
- Permanent Neurological Deficits: Damage to specific areas of the brain can result in long-term disabilities, such as paralysis or cognitive impairment.
- Death: In severe cases, the buildup of pressure can cause irreversible brain damage and death.
Early recognition and treatment are therefore critical to minimizing the risk of these complications and improving outcomes for affected individuals.