Ankylosing Spondylitis, commonly abbreviated as AS, is a chronic inflammatory condition that primarily affects the spine and sacroiliac joints. This condition belongs to a group of diseases known as spondyloarthropathies, which are characterized by inflammation in the joints and entheses (the sites where tendons and ligaments attach to bones). While Ankylosing Spondylitis predominantly impacts the spine, it can also affect other parts of the body, leading to a wide range of symptoms and complications. In this guide, we will explore the various aspects of this condition, including its symptoms, diagnostic methods, and available treatment options.
Understanding Ankylosing Spondylitis
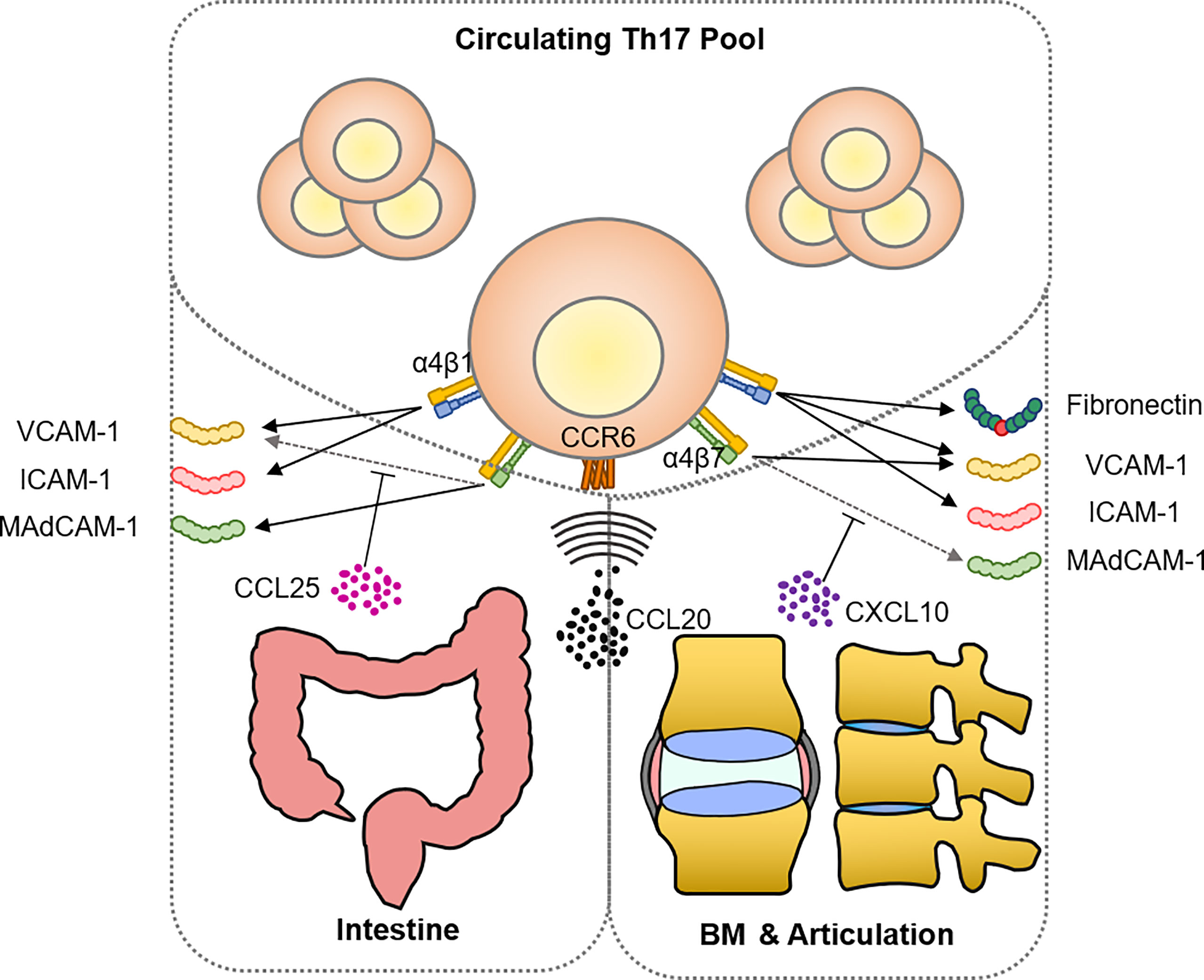
Ankylosing Spondylitis is an autoimmune disorder, meaning that the body’s immune system mistakenly attacks its own tissues. The exact cause of this condition remains unknown, but researchers believe that genetic and environmental factors play a significant role. One of the most well-known genetic markers associated with this condition is the HLA-B27 gene, although not everyone with this gene develops the disease.
This condition typically begins in early adulthood, often between the ages of 17 and 45, though it can occur at any age. It is more common in men than in women, and symptoms may vary in severity from person to person. Over time, untreated or poorly managed Ankylosing Spondylitis can lead to spinal fusion, where the vertebrae become rigid and immobile, causing a stooped posture and reduced flexibility.
Symptoms of Ankylosing Spondylitis
The symptoms of this condition can vary widely, and they often develop gradually over time. Some individuals may experience mild discomfort, while others may face severe pain and stiffness. Below are the most common symptoms associated with this condition:
- Chronic Back Pain: Persistent pain in the lower back and buttocks is one of the hallmark symptoms. This pain is often worse in the morning or after periods of inactivity and tends to improve with movement or exercise.
- Stiffness: Stiffness in the spine, particularly in the morning or after sitting for long periods, is another common symptom. This stiffness can make it difficult to perform daily activities.
- Fatigue: Many individuals with this condition report feeling unusually tired or fatigued, even after getting adequate rest.
- Pain in Other Joints: While the spine is the primary area affected, pain and swelling can also occur in other joints, such as the hips, shoulders, knees, and ankles.
- Enthesitis: Inflammation at the sites where tendons and ligaments attach to bones can cause pain in areas like the heels, ribs, or pelvis.
- Eyes Inflammation: Some people with this condition may develop uveitis or iritis, which are types of eye inflammation that can cause redness, pain, and blurred vision.
- Gastrointestinal Issues: There is a link between this condition and inflammatory bowel diseases like Crohn’s disease and ulcerative colitis, which can cause abdominal pain and digestive problems.
- Breathing Difficulties: As the disease progresses, the ribs may become stiff, making it harder to take deep breaths.
Diagnosing Ankylosing Spondylitis
Diagnosing this condition can be challenging because its symptoms often mimic those of other conditions, such as mechanical back pain or rheumatoid arthritis. Early diagnosis is crucial for effective management and preventing long-term complications. Below are the steps typically involved in diagnosing this condition:
Medical History and Physical Examination
A healthcare provider will begin by taking a detailed medical history and conducting a physical examination. They will ask about the nature of the pain, its duration, and any other symptoms you may be experiencing. During the physical exam, they may check for signs of restricted movement in the spine, pain during specific movements, and tenderness in certain areas.
Imaging Tests
Imaging tests are essential for confirming the presence of this condition. These tests help visualize the changes in the spine and sacroiliac joints caused by inflammation. Common imaging techniques include:
- X-rays: X-rays can reveal structural changes in the spine and sacroiliac joints, such as erosion or fusion of the vertebrae. However, these changes may not be visible in the early stages of the disease.
- Magnetic Resonance Imaging (MRI): MRI scans are more sensitive than X-rays and can detect early signs of inflammation in the joints and soft tissues. This makes MRI particularly useful for diagnosing this condition in its early stages.
Blood Tests
Blood tests are not definitive for diagnosing this condition, but they can provide supportive evidence. For example:
- HLA-B27 Test: The presence of the HLA-B27 gene is strongly associated with this condition, although not everyone with this gene develops the disease.
- Inflammatory Markers: Blood tests may show elevated levels of C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR), which indicate inflammation in the body.
Treatment Options for Ankylosing Spondylitis
While there is no cure for this condition, several treatment options are available to manage symptoms, slow disease progression, and improve quality of life. The treatment plan is often tailored to the individual’s specific needs and may involve a combination of medications, physical therapy, and lifestyle modifications.
Medications
Medications play a key role in managing the symptoms and reducing inflammation. Commonly prescribed medications include:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): These are often the first line of treatment and help relieve pain and stiffness. Examples include ibuprofen and naproxen.
- Disease-Modifying Antirheumatic Drugs (DMARDs): Medications like sulfasalazine may be prescribed if peripheral joints are affected.
- Biologic Therapies: Biologics, such as tumor necrosis factor (TNF) inhibitors, target specific components of the immune system to reduce inflammation. Examples include adalimumab and etanercept.
- Corticosteroids: In some cases, corticosteroid injections may be used to reduce inflammation in specific joints or areas of the body.
Physical Therapy and Exercise
Regular physical activity is essential for maintaining flexibility, improving posture, and reducing pain. A physical therapist can design a personalized exercise program that includes:
- Stretching Exercises: These help maintain or improve flexibility in the spine and other affected joints.
- Strengthening Exercises: Strengthening the core and back muscles can provide better support for the spine.
- Posture Training: Learning how to maintain proper posture can prevent the development of a stooped appearance.
- Low-Impact Aerobic Activities: Activities like swimming or walking can improve cardiovascular health without putting excessive strain on the joints.
Lifestyle Modifications
In addition to medications and physical therapy, certain lifestyle changes can help manage symptoms and improve overall well-being:
- Maintaining a Healthy Weight: Excess weight can put additional stress on the joints, worsening symptoms.
- Quitting Smoking: Smoking can accelerate the progression of this condition and increase the risk of complications.
- Using Proper Ergonomics: Adjusting workstations and using supportive chairs can reduce strain on the spine.
Surgical Interventions
In severe cases where joint damage has occurred, surgical interventions may be necessary. These procedures are typically reserved for individuals who do not respond to other treatments and may include:
- Joint Replacement Surgery: This involves replacing damaged joints, such as the hips or knees, with artificial ones.
- Osteotomy: This procedure involves cutting and realigning bones to improve posture and reduce pain.
Living with Ankylosing Spondylitis
Living with this condition requires a proactive approach to managing symptoms and maintaining a high quality of life. Regular follow-ups with healthcare providers, adherence to treatment plans, and staying informed about new developments in treatment options are essential. Support groups and counseling can also provide emotional support and practical advice for coping with the challenges of this condition.
By understanding the symptoms, seeking timely diagnosis, and exploring appropriate treatment options, individuals with this condition can effectively manage their symptoms and continue to lead fulfilling lives.