An ankle fracture, commonly referred to as a broken ankle, is a medical condition that occurs when one or more bones in the ankle joint are cracked or broken. The ankle joint is made up of three primary bones: the tibia, fibula, and talus. These bones work together to provide stability and support for walking, running, and other weight-bearing activities. When an injury disrupts this delicate balance, it can result in pain, swelling, and difficulty moving the foot. In this article, we will explore the different types of ankle fractures, their symptoms, how they are diagnosed, and the treatment options available.
Understanding the Anatomy of the Ankle
To fully grasp what happens during an ankle fracture, it is important to understand the anatomy of the ankle. The ankle joint is composed of three main bones:
- The tibia, which is the larger bone in the lower leg and forms the inner part of the ankle.
- The fibula, which is the smaller bone in the lower leg and forms the outer part of the ankle.
- The talus, which is the bone that connects the leg to the foot and allows for movement.
These bones are held together by ligaments, which are strong bands of tissue that provide stability to the joint. Any damage to these bones or ligaments can lead to a fracture or sprain, depending on the severity of the injury.
Types of Ankle Fractures
Ankle fractures can vary greatly in severity and location. They are typically classified based on which bones are affected and the extent of the damage. Below are some common types of ankle fractures:
1. Lateral Malleolus Fracture
This type of fracture involves the outer part of the ankle, specifically the fibula. It is one of the most common types of ankle fractures and often occurs due to twisting injuries or direct impact. Depending on the severity, the fracture may be stable or unstable.
2. Medial Malleolus Fracture
A medial malleolus fracture affects the inner part of the ankle, involving the tibia. This type of fracture is less common but can occur alongside other injuries, such as ligament tears. It is often caused by rotational forces or trauma.
3. Posterior Malleolus Fracture
This fracture involves the back part of the tibia, near the ankle joint. It is relatively uncommon but can occur in high-impact injuries. A posterior malleolus fracture may affect the stability of the ankle joint and is often associated with other fractures.
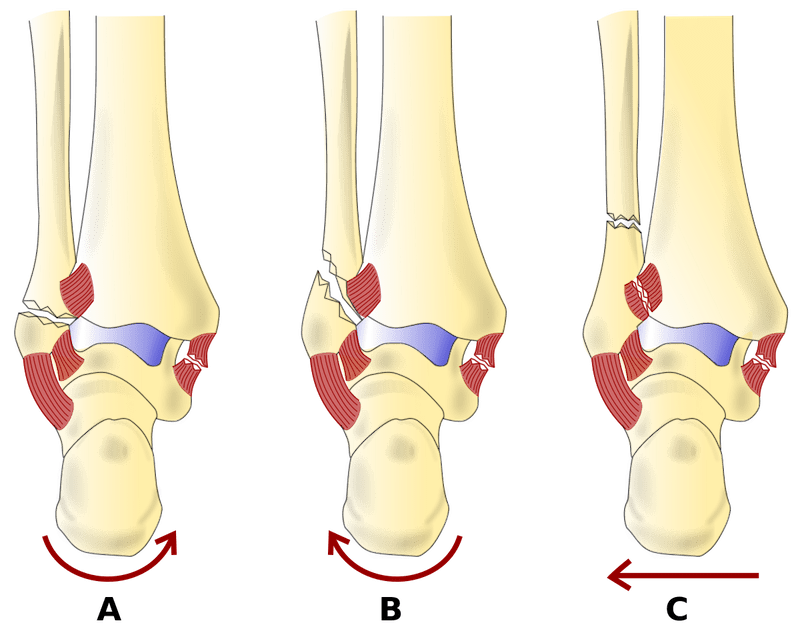
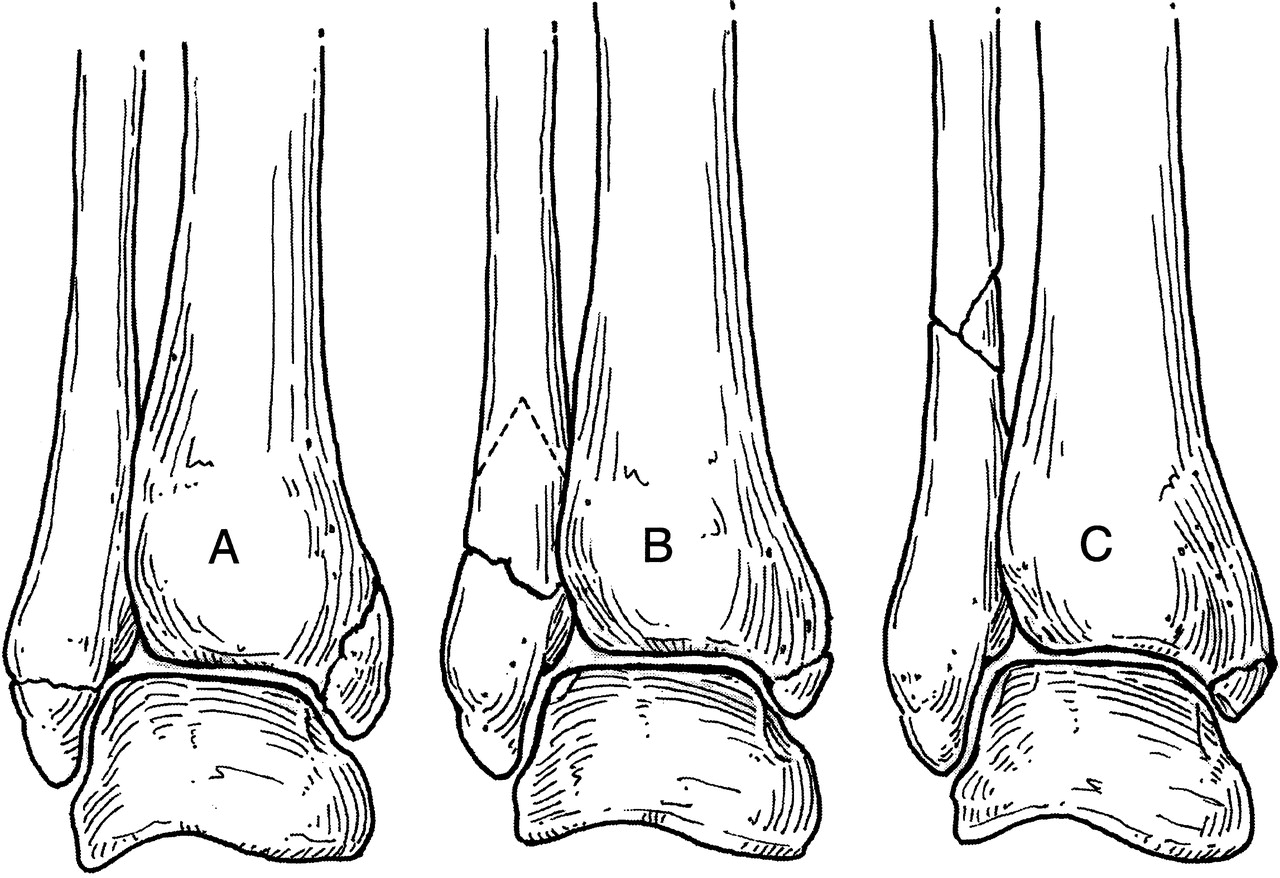
4. Bimalleolar Fracture
A bimalleolar fracture occurs when both the inner and outer parts of the ankle are broken. This type of injury is more severe and often requires surgical intervention. It is usually caused by significant trauma, such as a fall or car accident.
5. Trimalleolar Fracture
A trimalleolar fracture is a complex injury that involves all three parts of the ankle: the inner, outer, and back parts. This type of fracture is highly unstable and almost always requires surgery to repair.
6. Syndesmotic Injury
A syndesmotic injury occurs when the ligaments that connect the tibia and fibula are torn or stretched. While not a fracture itself, this injury often accompanies fractures and can significantly affect ankle stability.
Symptoms of an Ankle Fracture
The symptoms of an ankle fracture can vary depending on the severity of the injury. However, there are some common signs that may indicate a broken ankle:
- Severe pain that worsens with movement or weight-bearing.
- Swelling around the ankle joint.
- Bruising that may extend into the foot or lower leg.
- Tenderness to the touch, especially over the fractured area.
- Deformity or visible misalignment of the ankle.
- Inability to walk or bear weight on the affected leg.
- A popping or cracking sound at the time of injury.
If you experience any of these symptoms after an injury, it is important to seek medical attention promptly to determine the extent of the damage.
Diagnosis of an Ankle Fracture
Diagnosing an ankle fracture involves a combination of physical examination and imaging tests. Here is an overview of the diagnostic process:
1. Physical Examination
A healthcare provider will begin by examining the injured ankle. They will assess the level of pain, swelling, and bruising, as well as check for deformities or instability. The doctor may also ask about how the injury occurred and whether you are able to move your foot or bear weight.
2. X-rays
X-rays are the most common imaging test used to diagnose an ankle fracture. They provide detailed images of the bones and can help identify the location and severity of the fracture. In some cases, multiple X-rays may be taken from different angles to get a clearer picture.
3. Magnetic Resonance Imaging (MRI)
An MRI may be ordered if the X-rays do not provide enough information or if soft tissue damage, such as ligament tears, is suspected. This test uses magnetic fields and radio waves to create detailed images of the bones and surrounding tissues.
4. Computed Tomography (CT) Scan
A CT scan may be used to evaluate complex fractures or to get a more detailed view of the bone structure. This test combines multiple X-ray images to create a three-dimensional image of the ankle.
Treatment Options for an Ankle Fracture
The treatment for an ankle fracture depends on the type and severity of the injury. In general, treatment options can be divided into nonsurgical and surgical approaches.
Nonsurgical Treatment
Nonsurgical treatment is typically recommended for stable fractures that do not involve significant displacement of the bones. Common nonsurgical treatments include:
- Immobilization: The ankle may be placed in a cast, splint, or brace to keep the bones in place while they heal. This prevents further injury and promotes proper alignment.
- RICE Method: Rest, ice, compression, and elevation are often recommended to reduce pain and swelling during the initial stages of healing.
- Pain Management: Over-the-counter pain relievers, such as ibuprofen or acetaminophen, may be used to manage discomfort.
- Physical Therapy: Once the initial healing phase is complete, physical therapy may be recommended to restore strength, flexibility, and range of motion.
Surgical Treatment
Surgery is often required for unstable fractures, fractures involving multiple bones, or fractures that have shifted out of alignment. Surgical options include:
- Open Reduction and Internal Fixation (ORIF): This procedure involves realigning the bones and securing them in place with screws, plates, or rods. ORIF is commonly used for complex fractures.
- External Fixation: In some cases, an external frame may be used to stabilize the ankle. This involves inserting pins into the bones and connecting them to an external device.
- Ligament Repair: If ligaments are torn or damaged, they may need to be repaired or reconstructed during surgery.
Recovery and Rehabilitation
Recovery from an ankle fracture can take several weeks to months, depending on the severity of the injury. During this time, it is important to follow your healthcare provider’s instructions carefully to ensure proper healing. Rehabilitation exercises may be prescribed to improve strength and mobility, and crutches or a walker may be needed to avoid putting weight on the injured ankle.
Preventing Ankle Fractures
While not all ankle fractures can be prevented, there are steps you can take to reduce your risk of injury:
- Wear appropriate footwear for your activities, especially during sports or exercise.
- Warm up and stretch before engaging in physical activity.
- Be cautious on uneven surfaces to avoid trips and falls.
- Strengthen the muscles around the ankle through targeted exercises.
- Use protective gear, such as ankle braces, if you have a history of ankle injuries.
By taking these precautions, you can help protect your ankles and reduce the likelihood of sustaining a fracture.