An anal fistula, often abbreviated as AF, is a small tunnel that develops between the end of the bowel and the skin near the anus. This condition can cause significant discomfort and requires proper medical attention to prevent complications. In this article, we will explore the causes, symptoms, diagnosis, and treatments for anal fistulas in detail.
What Is an Anal Fistula?
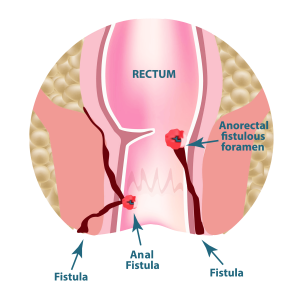
An anal fistula is an abnormal connection that forms between the anal canal or rectum and the skin surrounding the anus. These tunnels usually develop as a result of an infection in an anal gland. The infection leads to the formation of an abscess, which may eventually burst or require surgical drainage. If the abscess does not heal properly, it can lead to the development of a fistula.
Types of Anal Fistulas
- Intersphincteric Fistula: This is the most common type and occurs between the internal and external sphincter muscles.
- Transsphincteric Fistula: This type passes through both the internal and external sphincter muscles.
- Suprasphincteric Fistula: This fistula begins between the internal and external sphincter muscles but extends above the puborectalis muscle.
- Extrasphincteric Fistula: This rare type starts from the rectum or sigmoid colon and bypasses the sphincter muscles entirely.
Causes of Anal Fistulas
The primary cause of anal fistulas is an infection in one of the anal glands. However, several other factors can contribute to the development of this condition:
Infections
Infections in the anal glands are the leading cause of fistulas. When bacteria accumulate in these glands, they can form an abscess, which may later develop into a fistula if not treated properly.
Crohn’s Disease
Crohn’s disease, a chronic inflammatory condition of the gastrointestinal tract, increases the risk of developing anal fistulas. People with Crohn’s disease often experience inflammation in the lining of the digestive tract, which can affect the anal area.
Trauma or Surgery
Trauma to the anal region, including surgical procedures such as hemorrhoidectomy, can sometimes result in the formation of a fistula. Scarring and improper healing after surgery can also contribute to this condition.
Radiation Therapy
Patients who undergo radiation therapy for cancers in the pelvic region may develop anal fistulas as a side effect of the treatment. Radiation can damage tissues, leading to the formation of abnormal connections.
Tuberculosis
In rare cases, tuberculosis can affect the intestines and lead to the development of fistulas in the anal region. Tuberculosis-related fistulas are more commonly seen in regions where the disease is prevalent.
Symptoms of Anal Fistulas
Recognizing the symptoms of an anal fistula is crucial for early diagnosis and treatment. Some of the most common symptoms include:
Pain and Discomfort
Pain around the anus is one of the hallmark symptoms of an anal fistula. The pain may worsen when sitting, moving, or during bowel movements.
Swelling and Redness
The area around the anus may appear swollen and red. This swelling is often accompanied by tenderness and warmth, indicating the presence of an infection.
Discharge of Pus or Blood
A fistula may cause the discharge of pus or blood from an opening near the anus. This discharge can soil undergarments and cause irritation to the surrounding skin.
Fever
In some cases, individuals with an anal fistula may experience fever, especially if the condition is associated with an abscess or infection.
Irritation and Itching
The constant discharge from the fistula can irritate the skin around the anus, leading to itching and discomfort.
Diagnosis of Anal Fistulas
Diagnosing an anal fistula requires a thorough evaluation by a healthcare professional. Several diagnostic methods are used to confirm the presence of a fistula and determine its severity.
Physical Examination
A physical examination is often the first step in diagnosing an anal fistula. During this examination, the doctor will inspect the area around the anus for signs of swelling, redness, or discharge. They may also gently press on the area to check for pain or tenderness.
Anoscopy
An anoscopy involves inserting a small instrument called an anoscope into the anus to get a better view of the anal canal. This procedure helps the doctor identify the internal opening of the fistula and assess its depth and trajectory.
Magnetic Resonance Imaging
Magnetic resonance imaging, or MRI, is a non-invasive imaging technique that provides detailed images of the anal region. MRI scans are particularly useful for identifying complex fistulas and determining their relationship to the surrounding muscles and tissues.
Ultrasound
An ultrasound uses sound waves to create images of the internal structures of the body. In the case of anal fistulas, an endoanal ultrasound may be performed to visualize the fistula tract and its connection to the anal sphincter muscles.
Fistulography
Fistulography is a specialized X-ray procedure in which a contrast dye is injected into the fistula tract. This allows the doctor to see the path of the fistula and identify any branches or extensions.
Treatments for Anal Fistulas
Treatment for anal fistulas typically involves surgical intervention, as they rarely heal on their own. The goal of treatment is to eliminate the fistula while preserving the function of the anal sphincter muscles. Below are some of the most common treatment options:
Fistulotomy
A fistulotomy is the most common surgical procedure for treating simple anal fistulas. During this procedure, the surgeon cuts open the entire length of the fistula tract to allow it to heal from the inside out. Fistulotomy is effective for low fistulas that do not involve a significant portion of the sphincter muscles.
Seton Placement
For more complex or high fistulas, a seton may be placed. A seton is a piece of surgical thread that is inserted into the fistula tract to keep it open and allow for drainage. Over time, the seton helps the fistula heal gradually without causing damage to the sphincter muscles.
Advancement Flap Procedure
The advancement flap procedure involves covering the internal opening of the fistula with a flap of tissue taken from the rectum or anus. This technique is often used for high fistulas to reduce the risk of incontinence.
LIFT Procedure
The ligation of the intersphincteric fistula tract, or LIFT procedure, is a newer surgical technique designed to treat complex fistulas. During this procedure, the surgeon accesses the fistula tract between the sphincter muscles and ties it off to promote healing.
Fibrin Glue Injection
Fibrin glue injection is a minimally invasive treatment option for certain types of fistulas. The surgeon injects a special glue into the fistula tract to seal it shut. While this method is less invasive, it may not be as effective for complex or recurrent fistulas.
Bioprosthetic Plug
A bioprosthetic plug is a cone-shaped device made from animal tissue that is inserted into the fistula tract. The plug promotes healing by encouraging the growth of new tissue around it. This method is still being studied for its long-term effectiveness.
Antibiotics and Pain Management
In addition to surgical treatments, antibiotics may be prescribed to manage infections associated with the fistula. Pain management strategies, including over-the-counter or prescription medications, are also important for ensuring patient comfort during recovery.
Lifestyle and Home Remedies
While medical and surgical treatments are essential for managing anal fistulas, certain lifestyle changes and home remedies can help alleviate symptoms and support healing:
Dietary Adjustments
Eating a high-fiber diet can help soften stools and reduce strain during bowel movements. This can minimize irritation to the anal area and promote faster healing.
Sitz Baths
Taking warm sitz baths several times a day can provide relief from pain and discomfort. Soaking the affected area in warm water also helps keep the area clean and reduces the risk of infection.
Hygiene Practices
Maintaining good hygiene is crucial for preventing complications. Gently cleaning the anal area with mild soap and water after bowel movements can help prevent irritation and infection.
Avoiding Straining
Avoiding activities that put pressure on the anal area, such as heavy lifting or prolonged sitting, can aid in the healing process. It is also important to avoid straining during bowel movements.
When to See a Doctor
If you experience persistent pain, swelling, or discharge around the anus, it is important to seek medical attention promptly. Early diagnosis and treatment can prevent complications and improve outcomes. Additionally, individuals with underlying conditions such as Crohn’s disease should consult their healthcare provider regularly to monitor for signs of fistula development.





