Irritable Bowel Syndrome, commonly abbreviated as IBS, is a chronic gastrointestinal disorder that affects millions of people worldwide. It is characterized by a group of symptoms that typically occur together, including abdominal pain, bloating, and changes in bowel habits. Unlike other digestive disorders, this condition does not cause visible damage to the intestines but can significantly impact a person’s quality of life. Understanding its symptoms, identifying triggers, and exploring management options are essential steps toward living well with this condition.
Understanding the Symptoms
The symptoms of Irritable Bowel Syndrome can vary widely from person to person, making it a challenging condition to diagnose. However, there are some common signs that many individuals with this condition experience:
- Abdominal Pain or Discomfort: One of the hallmark symptoms is recurring pain or discomfort in the abdomen. This pain often improves after a bowel movement.
- Bloating and Gas: Many people report feeling bloated or swollen in the abdomen, accompanied by excessive gas production.
- Changes in Bowel Habits: Some individuals experience diarrhea, while others may have constipation. In some cases, both symptoms alternate.
- Mucus in Stool: The presence of mucus in the stool is another common symptom associated with this condition.
- Fatigue and Difficulty Sleeping: Many individuals report feeling unusually tired or having trouble sleeping due to the discomfort caused by their symptoms.
It is important to note that these symptoms can fluctuate over time, with periods of relief followed by flare-ups. Keeping track of these patterns can help individuals better understand their condition and work with healthcare providers to manage it effectively.
Identifying Common Triggers
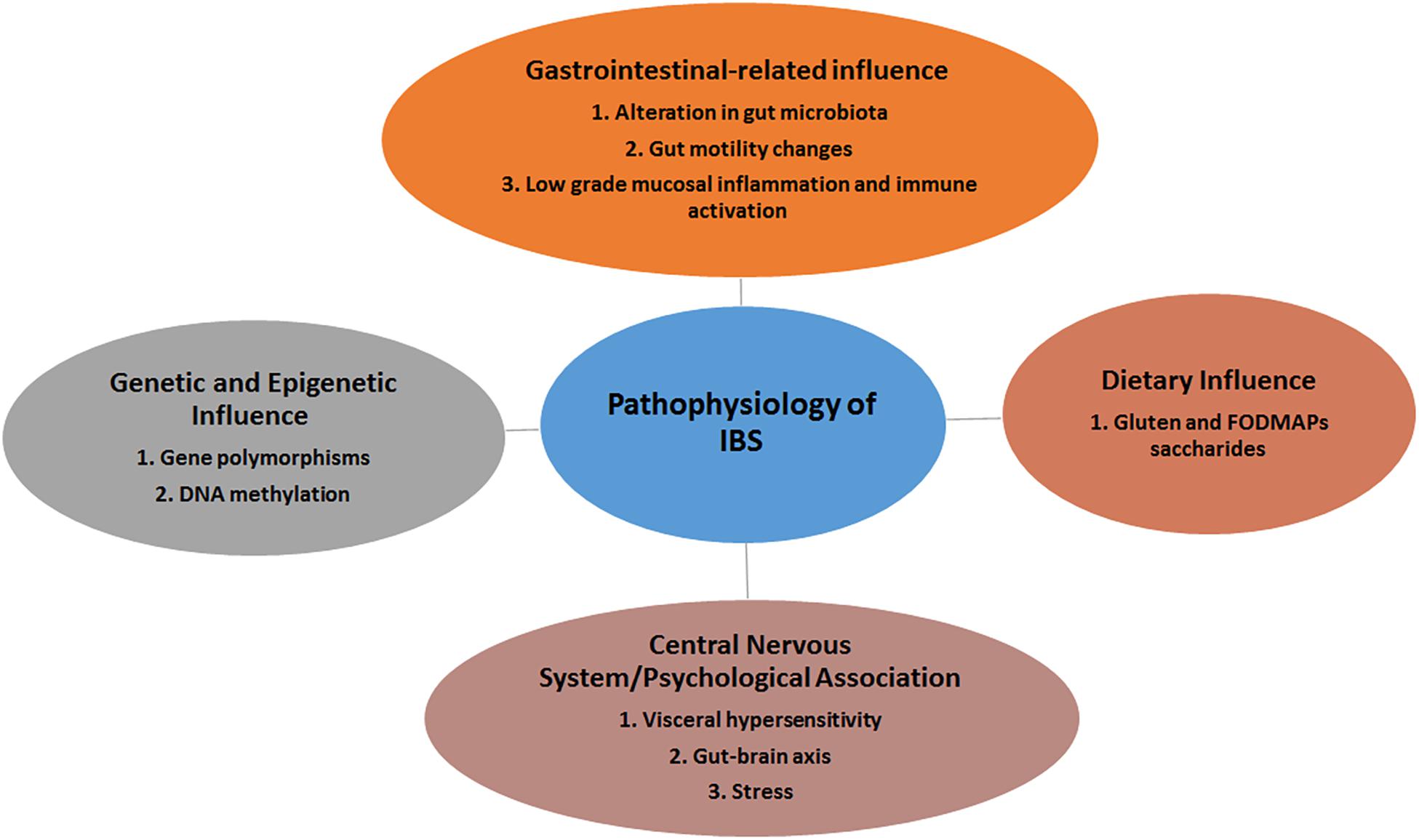
While the exact cause of Irritable Bowel Syndrome remains unknown, certain factors are known to trigger or worsen its symptoms. Identifying and avoiding these triggers can play a significant role in managing the condition. Below are some of the most common triggers:
Dietary Factors
Certain foods and beverages are known to exacerbate symptoms in many individuals. These include:
- Fatty Foods: High-fat meals can be difficult to digest and may lead to discomfort.
- Dairy Products: Lactose intolerance is common among people with this condition, leading to bloating and diarrhea.
- Carbonated Drinks: Beverages like soda can increase gas production and contribute to bloating.
- Caffeine and Alcohol: Both substances can irritate the digestive system and worsen symptoms.
- High-Fiber Foods: While fiber is generally beneficial for digestion, some high-fiber foods, such as beans and certain vegetables, may cause gas and bloating in sensitive individuals.
Stress and Anxiety
Emotional stress and anxiety are closely linked to the severity of symptoms in people with this condition. The gut-brain connection plays a significant role, as stress can disrupt normal digestive processes and lead to flare-ups. Managing stress through relaxation techniques, therapy, or mindfulness practices can help reduce symptom frequency and intensity.
Hormonal Changes
Many women with this condition report that their symptoms worsen during their menstrual cycle. Hormonal fluctuations may influence gut motility and sensitivity, contributing to increased discomfort during these times.
Medications and Supplements
Certain medications, such as antibiotics or nonsteroidal anti-inflammatory drugs, can irritate the digestive tract and trigger symptoms. Additionally, some dietary supplements, particularly those containing artificial sweeteners or high doses of certain vitamins, may also act as triggers.
Management Options
While there is no cure for this condition, several strategies can help manage symptoms and improve overall well-being. A combination of dietary adjustments, lifestyle changes, and medical treatments is often the most effective approach.
Dietary Modifications
One of the first steps in managing symptoms is making dietary changes. Working with a registered dietitian can help individuals identify which foods to avoid and which to incorporate into their diet. Some popular dietary approaches include:
- Low FODMAP Diet: This diet focuses on reducing the intake of fermentable carbohydrates that can cause bloating and gas. Foods high in FODMAPs include certain fruits, vegetables, grains, and dairy products.
- Increase Soluble Fiber Intake: Soluble fiber, found in foods like oats and carrots, can help regulate bowel movements without causing excessive gas.
- Stay Hydrated: Drinking plenty of water supports healthy digestion and helps prevent constipation.
Lifestyle Changes
In addition to dietary modifications, certain lifestyle changes can make a significant difference in managing symptoms:
- Exercise Regularly: Physical activity can help regulate bowel movements and reduce stress levels.
- Prioritize Sleep: Poor sleep can exacerbate symptoms, so establishing a consistent sleep routine is essential.
- Practice Stress Management Techniques: Activities such as yoga, meditation, and deep breathing exercises can help reduce stress and improve gut health.
Medical Treatments
For individuals whose symptoms are not adequately controlled through lifestyle and dietary changes, medical treatments may be necessary. These treatments often focus on alleviating specific symptoms:
- Antispasmodic Medications: These drugs help relax the muscles in the digestive tract, reducing cramping and pain.
- Laxatives: For those experiencing constipation, over-the-counter or prescription laxatives may provide relief.
- Antidiarrheal Medications: Over-the-counter options like loperamide can help control diarrhea.
- Probiotics: Some studies suggest that probiotics, which promote the growth of beneficial gut bacteria, may help alleviate symptoms in certain individuals.
Alternative Therapies
Some people find relief through alternative therapies, although scientific evidence supporting their effectiveness varies. These therapies include:
- Acupuncture: This traditional Chinese medicine practice involves inserting thin needles into specific points on the body and may help reduce pain and stress.
- Hypnotherapy: Gut-directed hypnotherapy has been shown to improve symptoms in some individuals by addressing the gut-brain connection.
- Herbal Remedies: Certain herbs, such as peppermint oil, are believed to have calming effects on the digestive system.
Working with Healthcare Providers
Managing this condition often requires a collaborative approach between individuals and their healthcare providers. Open communication about symptoms, triggers, and treatment preferences is key to developing an effective management plan. Regular check-ins with a primary care physician or gastroenterologist can help monitor progress and make necessary adjustments to the treatment plan.
In some cases, additional testing may be required to rule out other conditions with similar symptoms, such as inflammatory bowel disease or celiac disease. A thorough evaluation ensures that individuals receive the most appropriate care for their specific needs.
Support and Community Resources
Living with this condition can feel isolating, but connecting with others who share similar experiences can provide valuable support. Online forums, local support groups, and educational resources offer opportunities to learn from others and share coping strategies. Engaging with a community can also help reduce feelings of stigma and empower individuals to take an active role in managing their health.
Final Thoughts
While living with this condition presents challenges, understanding its symptoms, identifying triggers, and exploring management options can significantly improve quality of life. By adopting a proactive approach and working closely with healthcare providers, individuals can gain greater control over their symptoms and achieve a better sense of well-being.