Ischemic cardiomyopathy, often abbreviated as ICM, is a condition that affects the heart’s ability to pump blood effectively due to damage caused by reduced blood flow. This condition is one of the leading causes of heart failure and can significantly impact a person’s quality of life. In this article, we will explore ischemic cardiomyopathy in detail, including its causes, symptoms, and available treatments.
What is Ischemic Cardiomyopathy?
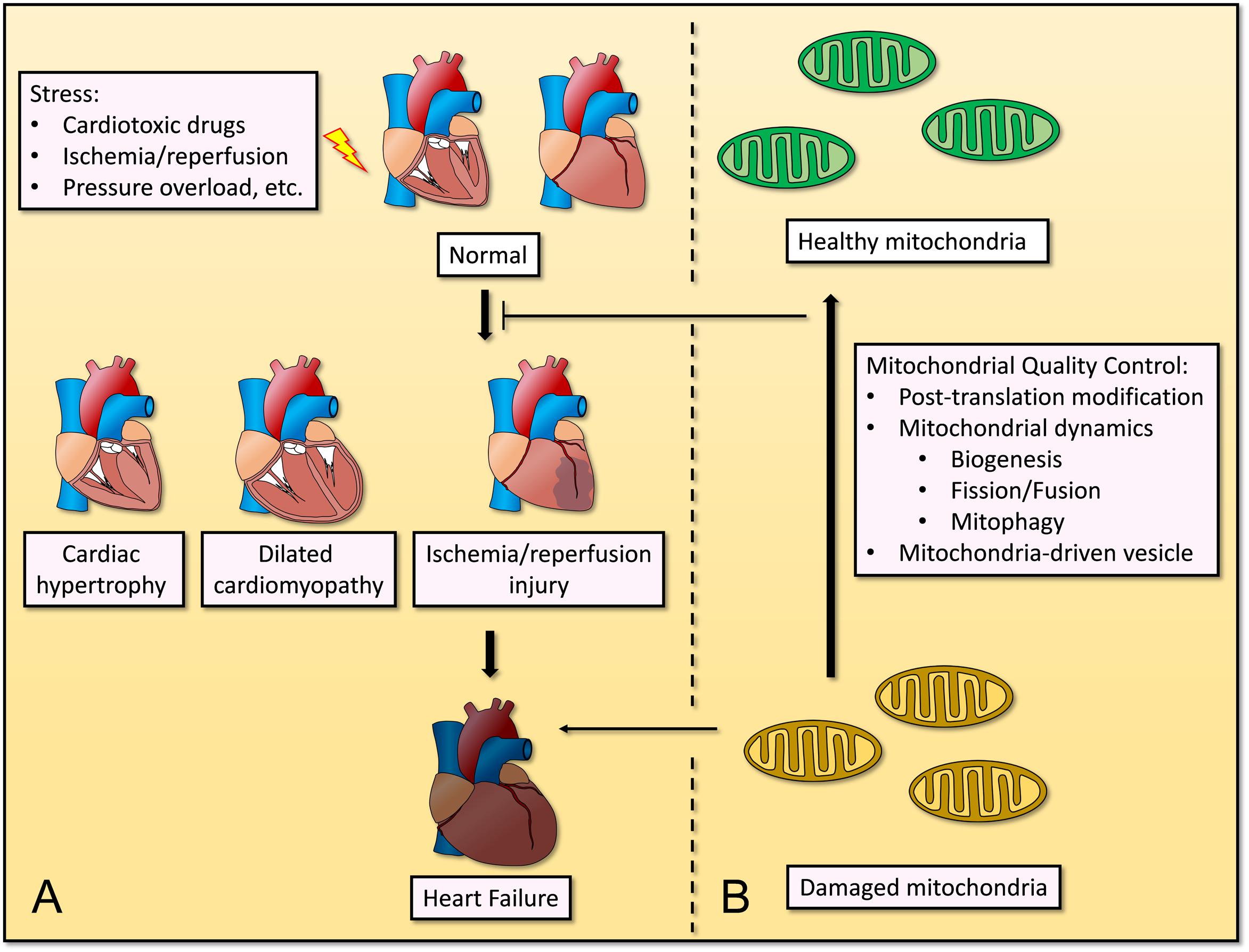
Ischemic cardiomyopathy occurs when the heart muscle becomes weakened due to insufficient blood supply. The lack of adequate blood flow is typically caused by coronary artery disease, which involves the narrowing or blockage of the arteries that supply oxygen-rich blood to the heart. Over time, this reduced blood flow can lead to the death of heart muscle tissue, impairing the heart’s ability to pump blood efficiently.
How Does It Differ from Other Types of Cardiomyopathy?
- Dilated Cardiomyopathy: This condition involves the enlargement of the heart chambers, leading to weakened pumping ability. Unlike ischemic cardiomyopathy, it is not necessarily caused by blocked arteries.
- Hypertrophic Cardiomyopathy: This condition is characterized by the thickening of the heart muscle, which can obstruct blood flow. It is often genetic and unrelated to coronary artery disease.
- Restrictive Cardiomyopathy: This rare form involves the stiffening of the heart muscle, making it difficult for the heart to fill with blood. It is not directly linked to coronary artery disease.
Causes of Ischemic Cardiomyopathy
The primary cause of ischemic cardiomyopathy is coronary artery disease. However, several factors contribute to the development of this condition. Understanding these causes can help in prevention and early intervention.
Coronary Artery Disease
Coronary artery disease occurs when fatty deposits, known as plaques, build up on the walls of the coronary arteries. These plaques narrow the arteries, reducing blood flow to the heart muscle. If a plaque ruptures, it can lead to the formation of a blood clot, which may completely block the artery and cause a heart attack. Repeated episodes of reduced blood flow or heart attacks can weaken the heart muscle, leading to ischemic cardiomyopathy.
Risk Factors
- High Blood Pressure: Elevated blood pressure puts extra strain on the heart, increasing the risk of coronary artery disease.
- High Cholesterol Levels: Excess cholesterol can contribute to the buildup of plaques in the arteries.
- Smoking: Smoking damages the lining of the arteries, making them more susceptible to plaque buildup.
- Diabetes: High blood sugar levels can damage blood vessels and increase the risk of coronary artery disease.
- Obesity: Excess weight can contribute to high blood pressure, high cholesterol, and diabetes, all of which are risk factors for coronary artery disease.
- Family History: A family history of heart disease increases the likelihood of developing ischemic cardiomyopathy.
Symptoms of Ischemic Cardiomyopathy
The symptoms of ischemic cardiomyopathy often develop gradually and may be mistaken for other conditions. Recognizing these symptoms early can help in seeking timely medical intervention.
Common Symptoms
- Shortness of Breath: Difficulty breathing, especially during physical activity or while lying down, is a common symptom. This occurs because the heart cannot pump enough blood to meet the body’s needs.
- Fatigue: Feeling tired or weak, even after minimal exertion, is another sign of reduced heart function.
- Swelling: Swelling in the legs, ankles, feet, or abdomen may occur due to fluid retention, a condition known as edema.
- Chest Pain: Chest discomfort or pain, also known as angina, may occur when the heart does not receive enough oxygen-rich blood.
- Irregular Heartbeat: Palpitations or an irregular heartbeat can indicate that the heart is struggling to maintain normal function.
- Dizziness or Fainting: Reduced blood flow to the brain can cause dizziness or fainting spells.
When to Seek Medical Attention
If you experience any of the following symptoms, it is important to seek medical attention immediately:
- Chest pain that lasts more than a few minutes
- Severe shortness of breath
- Fainting or near-fainting episodes
- Rapid or irregular heartbeat accompanied by dizziness
Treatments for Ischemic Cardiomyopathy
Treatment for ischemic cardiomyopathy focuses on managing symptoms, improving heart function, and preventing further damage. The approach may involve lifestyle changes, medications, and surgical procedures, depending on the severity of the condition.
Lifestyle Modifications
Making healthy lifestyle choices is essential for managing ischemic cardiomyopathy. These changes can help reduce the workload on the heart and improve overall health.
- Healthy Diet: Consuming a diet rich in fruits, vegetables, whole grains, and lean proteins can help lower cholesterol and blood pressure.
- Regular Exercise: Engaging in moderate physical activity, as recommended by a healthcare provider, can strengthen the heart and improve circulation.
- Weight Management: Maintaining a healthy weight reduces the strain on the heart and lowers the risk of complications.
- Smoking Cessation: Quitting smoking is crucial for improving heart health and preventing further damage to the arteries.
- Stress Management: Techniques such as meditation, yoga, or counseling can help reduce stress, which may otherwise exacerbate heart problems.
Medications
Several medications are commonly prescribed to manage ischemic cardiomyopathy and its symptoms. These medications work by improving heart function, reducing fluid retention, and controlling underlying conditions such as high blood pressure or diabetes.
- Beta-Blockers: These medications slow the heart rate and reduce the workload on the heart, helping it pump more efficiently.
- ACE Inhibitors: Angiotensin-converting enzyme inhibitors help relax blood vessels, lowering blood pressure and improving blood flow.
- Diuretics: Also known as water pills, diuretics help reduce fluid retention and relieve symptoms such as swelling and shortness of breath.
- Antiplatelet Drugs: Medications like aspirin prevent blood clots from forming, reducing the risk of heart attacks.
- Statins: These drugs lower cholesterol levels, slowing the progression of coronary artery disease.
Surgical Procedures
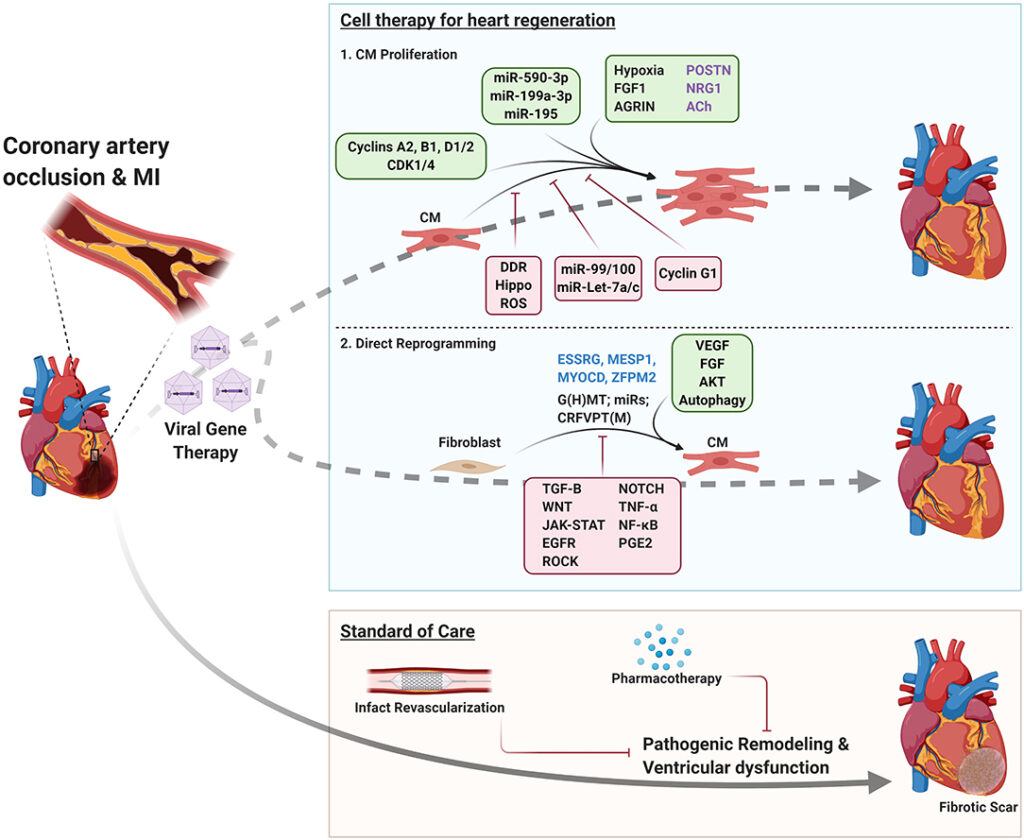
In cases where medications and lifestyle changes are not sufficient, surgical interventions may be necessary to restore blood flow to the heart and improve its function.
- Coronary Artery Bypass Grafting: This procedure involves using a healthy blood vessel from another part of the body to bypass a blocked artery, restoring blood flow to the heart muscle.
- Angioplasty and Stenting: During angioplasty, a small balloon is used to widen a narrowed artery. A stent may then be placed to keep the artery open.
- Implantable Devices: Devices such as pacemakers or implantable cardioverter-defibrillators can help regulate the heartbeat and prevent life-threatening arrhythmias.
- Heart Transplant: In severe cases where the heart is irreversibly damaged, a heart transplant may be considered as a last resort.
Cardiac Rehabilitation
Cardiac rehabilitation programs are designed to help individuals recover from heart-related conditions and improve their overall cardiovascular health. These programs typically include supervised exercise, education on heart-healthy living, and emotional support.
Prevention of Ischemic Cardiomyopathy
While some risk factors for ischemic cardiomyopathy, such as family history, cannot be changed, many others can be managed through proactive measures. Preventive strategies focus on reducing the risk of coronary artery disease and maintaining a healthy heart.
- Adopting a heart-healthy diet low in saturated fats, salt, and processed foods
- Engaging in regular physical activity to strengthen the heart and improve circulation
- Monitoring and managing conditions such as high blood pressure, high cholesterol, and diabetes
- Avoiding tobacco use and limiting alcohol consumption
- Attending regular check-ups with a healthcare provider to monitor heart health