Intestinal obstruction, commonly referred to as ileus, is a medical condition that disrupts the normal movement of the contents within the intestines. This disruption can lead to severe complications if not addressed promptly. Ileus affects people of all ages and requires careful diagnosis and treatment. In this article, we will explore the causes, symptoms, and available treatments for this condition.
Understanding Ileus
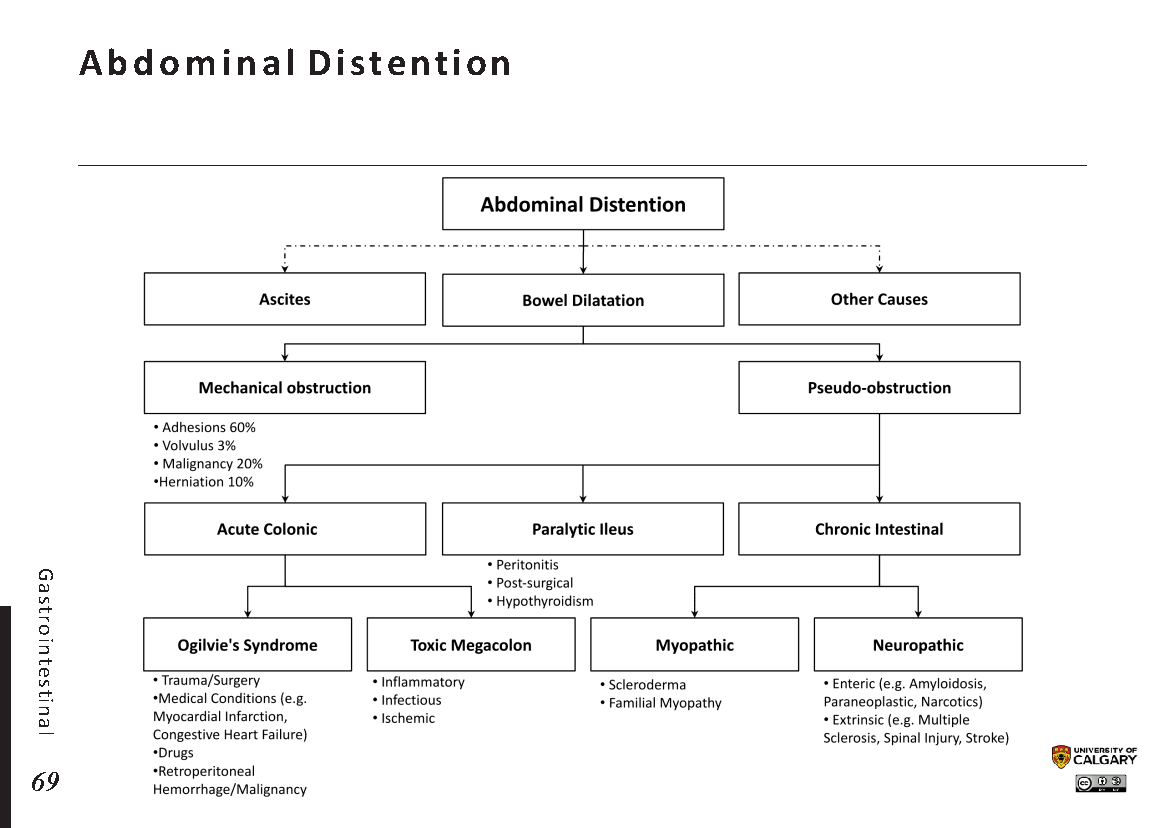
Ileus occurs when the intestines fail to contract properly, leading to a slowdown or complete halt in the movement of food, fluids, and gas through the digestive tract. Unlike mechanical obstructions, where a physical blockage prevents the passage of intestinal contents, ileus is often caused by issues related to muscle or nerve function. The result is a functional obstruction rather than a structural one.
Types of Ileus
- Paralytic Ileus: This is the most common type and occurs when the muscles of the intestines become temporarily paralyzed. It is often seen after abdominal surgery or due to certain medications.
- Adynamic Ileus: Similar to paralytic ileus, adynamic ileus refers to a lack of intestinal motility but is typically associated with more chronic conditions like severe infections or metabolic disorders.
- Spastic Ileus: In this rare form, the muscles of the intestines contract excessively, leading to cramping and discomfort without any actual blockage.
Causes of Ileus
The development of ileus can be attributed to various factors, ranging from surgical procedures to underlying health conditions. Below are some of the primary causes:
Post-Surgical Effects
One of the most common triggers for ileus is surgery, particularly abdominal or pelvic surgeries. During these procedures, the intestines may become temporarily “stunned” due to manipulation or inflammation, leading to reduced motility. Anesthesia and pain medications administered during surgery can also contribute to this condition.
Medications
Certain medications are known to slow down intestinal activity. Opioids, which are often prescribed for pain relief, are a frequent culprit. Antidepressants, anticholinergics, and medications used to treat high blood pressure can also interfere with normal intestinal function.
Infections and Inflammation
Infections such as gastroenteritis or appendicitis can irritate the lining of the intestines, causing them to stop functioning properly. Similarly, inflammatory conditions like Crohn’s disease or ulcerative colitis can lead to ileus by affecting the nerves and muscles of the digestive tract.
Metabolic Imbalances
Electrolyte imbalances, such as low levels of potassium or magnesium, can disrupt the electrical signals that control muscle contractions in the intestines. Other metabolic issues, including kidney failure or diabetes, may also contribute to the development of ileus.
Trauma
Physical trauma to the abdomen, whether from an accident or injury, can damage the intestines or surrounding tissues. This damage can impair the normal movement of the digestive system, resulting in ileus.
Symptoms of Ileus
The symptoms of ileus can vary depending on the severity of the condition and its underlying cause. However, there are several common signs that individuals may experience:
Abdominal Pain and Cramping
Pain in the abdomen is one of the hallmark symptoms of ileus. The discomfort is often described as cramp-like and may come and go. In some cases, the pain can be severe and constant, especially if the condition worsens.
Bloating and Swelling
As the intestines fail to move their contents forward, gas and fluid can build up, leading to bloating and visible swelling of the abdomen. This distension can cause additional discomfort and make it difficult for the individual to eat or drink.
Nausea and Vomiting
When the intestines are unable to process food and fluids, nausea and vomiting often occur. The vomit may contain bile, indicating that the blockage is affecting the upper part of the digestive tract.
Constipation
A lack of bowel movements is another key symptom of ileus. Individuals may notice that they are unable to pass stool or gas, which can further exacerbate feelings of discomfort and bloating.
Lack of Appetite
Due to the discomfort and bloating associated with ileus, many individuals lose their appetite. This can lead to dehydration and malnutrition if the condition persists for an extended period.
Diagnosis of Ileus
Diagnosing ileus involves a combination of physical examinations, medical history reviews, and diagnostic tests. Healthcare providers will typically follow these steps:
Physical Examination
A healthcare provider will begin by examining the abdomen for signs of swelling, tenderness, or unusual sounds. They may also listen to the abdomen using a stethoscope to check for the presence or absence of bowel sounds, which can indicate reduced intestinal activity.
Imaging Tests
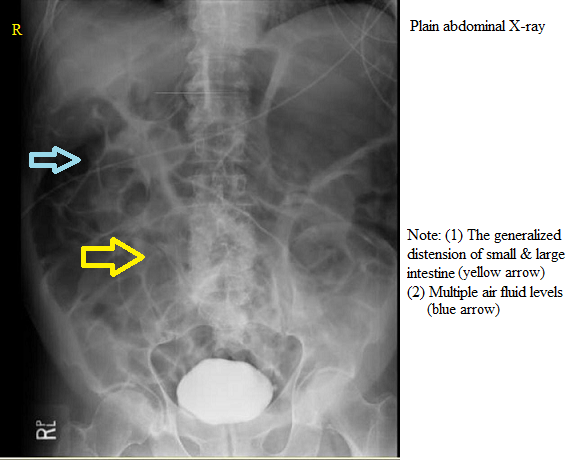
Imaging studies are crucial for confirming the diagnosis of ileus. Common tests include:
- X-rays: These can reveal the presence of gas or fluid buildup in the intestines.
- CT Scans: Computed tomography scans provide detailed images of the abdomen and can help rule out mechanical obstructions.
- Ultrasound: This non-invasive test is often used to assess the movement of the intestines and identify areas of concern.
Blood Tests
Blood tests may be conducted to check for signs of infection, electrolyte imbalances, or other underlying conditions that could be contributing to the development of ileus.
Treatment Options for Ileus
The treatment of ileus depends on its underlying cause and severity. In most cases, the goal is to restore normal intestinal function and prevent complications. Below are some of the common treatment approaches:
Conservative Management
For mild cases of ileus, conservative management is often sufficient. This approach includes:
- Bowel Rest: Patients are advised to avoid eating solid foods for a period of time to allow the intestines to recover. Intravenous fluids may be administered to prevent dehydration.
- Nasogastric Decompression: A tube may be inserted through the nose into the stomach to remove excess gas and fluid, relieving pressure in the intestines.
- Medication Adjustment: If medications are contributing to the condition, healthcare providers may adjust dosages or switch to alternative treatments.
Addressing Underlying Conditions
If ileus is caused by an underlying condition, such as an infection or metabolic imbalance, treating that condition is essential. For example:
- Infection Treatment: Antibiotics may be prescribed to address bacterial infections.
- Electrolyte Correction: Intravenous solutions may be used to restore proper electrolyte levels.
Surgical Intervention
In severe cases where conservative measures fail or if there is evidence of complications such as tissue death or perforation, surgery may be necessary. Surgical options include:
- Removal of Obstructions: If a partial mechanical obstruction is present, it may need to be removed surgically.
- Repair of Damage: Surgery may be required to repair damaged tissues or address complications like abscesses.
Lifestyle Modifications
After recovering from ileus, individuals may be advised to make certain lifestyle changes to reduce the risk of recurrence. These may include:
- Dietary Adjustments: Consuming a high-fiber diet and staying hydrated can promote healthy digestion.
- Exercise: Regular physical activity can help stimulate intestinal motility.
- Medication Review: Working with healthcare providers to minimize the use of medications that affect intestinal function.
Complications of Untreated Ileus
If left untreated, ileus can lead to serious complications, including:
- Perforation: The buildup of pressure in the intestines can cause the walls to rupture, leading to life-threatening infections.
- Tissue Death: Prolonged lack of blood flow to the intestines can result in tissue death, requiring surgical intervention.
- Sepsis: Infections that spread throughout the body can lead to sepsis, a potentially fatal condition.
Preventing Ileus
While not all cases of ileus can be prevented, certain measures can reduce the risk:
- Early Ambulation After Surgery: Walking soon after surgery can help stimulate intestinal activity.
- Proper Medication Use: Using medications only as directed and discussing alternatives with healthcare providers can minimize risks.
- Managing Chronic Conditions: Keeping conditions like diabetes or inflammatory bowel disease under control can help prevent complications.