Hypereosinophilic Syndrome, often abbreviated as HES, is a rare and complex medical condition characterized by an abnormally high number of eosinophils in the blood. Eosinophils are a type of white blood cell that plays a crucial role in the immune system, particularly in fighting infections and responding to allergens. However, when their levels rise excessively and persistently without a clear cause, it can lead to widespread tissue damage and organ dysfunction. In this article, we will explore the causes, symptoms, and available treatments for this challenging condition.
Understanding Hypereosinophilic Syndrome
Hypereosinophilic Syndrome is not a single disease but rather a group of disorders that share a common feature: an overproduction of eosinophils. These cells, when present in excessive numbers, infiltrate various organs and tissues, causing inflammation and damage. The syndrome can affect multiple systems in the body, including the heart, lungs, skin, nervous system, and digestive tract. Because of its systemic nature, diagnosing and managing this condition requires a multidisciplinary approach.
What Are Eosinophils?
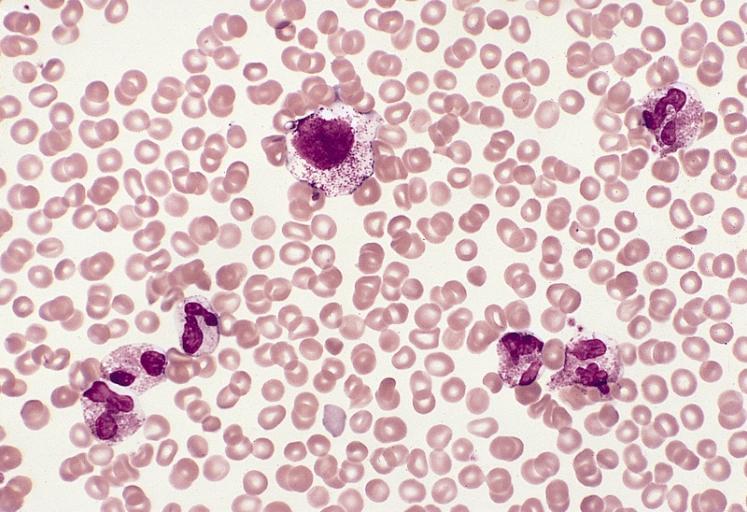
Eosinophils are a subtype of white blood cells that are part of the body’s immune response. They help fight off infections caused by parasites and play a role in allergic reactions. Normally, eosinophils make up only a small percentage of the total white blood cell count. However, in cases of Hypereosinophilic Syndrome, their numbers increase significantly, sometimes reaching levels that are hundreds or even thousands of times higher than normal.
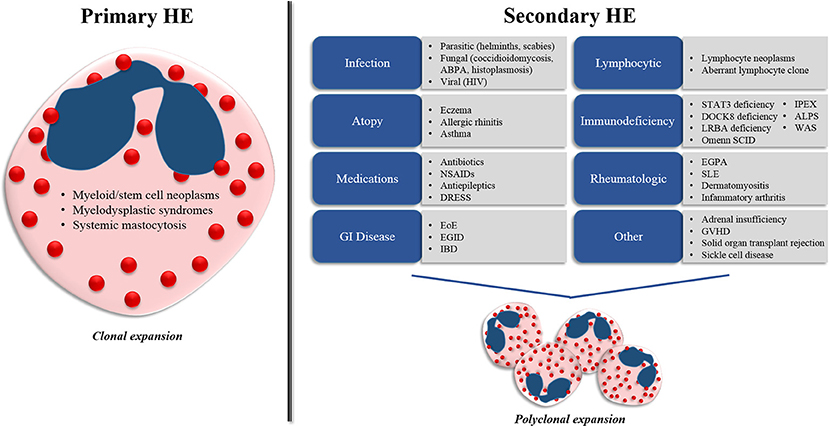
Causes of Hypereosinophilic Syndrome
The exact cause of Hypereosinophilic Syndrome is not always clear, and in many cases, it remains unknown. However, researchers have identified several potential factors that may contribute to the development of this condition. These include genetic mutations, autoimmune responses, and underlying diseases.
Genetic Mutations
In some patients, Hypereosinophilic Syndrome is linked to specific genetic mutations. One of the most well-known mutations occurs in the FIP1L1-PDGFRA gene fusion, which leads to the overproduction of eosinophils. This mutation is often associated with a subtype of the syndrome that responds well to certain medications. Identifying such genetic abnormalities is critical for tailoring treatment plans to individual patients.
Autoimmune Disorders
- Lupus: Systemic lupus erythematosus, an autoimmune disease, has been linked to elevated eosinophil counts in some cases.
- Rheumatoid Arthritis: Chronic inflammatory conditions like rheumatoid arthritis can also trigger eosinophilia.
- Allergies: Severe allergic reactions or chronic allergic conditions may contribute to the overproduction of eosinophils.
Underlying Diseases
Hypereosinophilic Syndrome can also be secondary to other medical conditions. For example, parasitic infections, certain cancers like lymphoma, and even some medications can cause eosinophil levels to rise. In these cases, treating the underlying condition often helps resolve the eosinophilia.
Symptoms of Hypereosinophilic Syndrome
The symptoms of Hypereosinophilic Syndrome vary widely depending on which organs are affected. Some patients may experience mild symptoms, while others develop severe complications. Early recognition of these symptoms is essential for timely diagnosis and treatment.
Cardiac Symptoms
One of the most serious complications of Hypereosinophilic Syndrome involves the heart. Eosinophils can infiltrate the heart muscle, leading to inflammation and scarring. This can result in conditions such as:
- Heart failure
- Arrhythmias (irregular heartbeats)
- Endocarditis (inflammation of the inner lining of the heart)
Pulmonary Symptoms
When eosinophils accumulate in the lungs, they can cause respiratory issues. Common pulmonary symptoms include:
- Shortness of breath
- Coughing
- Wheezing
- Chest pain
Skin Manifestations
Skin involvement is another hallmark of Hypereosinophilic Syndrome. Patients may notice rashes, hives, or itching. In some cases, the skin lesions can become painful or disfiguring.
Gastrointestinal Symptoms
The digestive system can also be affected, leading to symptoms such as:
- Abdominal pain
- Nausea and vomiting
- Diarrhea
- Difficulty swallowing
Neurological Symptoms
When eosinophils infiltrate the nervous system, patients may experience:
- Peripheral neuropathy (numbness or tingling in the extremities)
- Seizures
- Confusion or memory problems
Diagnosing Hypereosinophilic Syndrome
Diagnosing Hypereosinophilic Syndrome can be challenging because its symptoms mimic those of many other conditions. A thorough evaluation is necessary to rule out other potential causes of eosinophilia.
Blood Tests
Blood tests are the first step in diagnosing this condition. A complete blood count will reveal elevated eosinophil levels. Further testing, such as bone marrow biopsy, may be required to confirm the diagnosis and identify any underlying causes.
Imaging Studies
Imaging studies like echocardiograms, chest X-rays, and CT scans can help assess the extent of organ involvement. For example, an echocardiogram can detect signs of heart damage caused by eosinophil infiltration.
Genetic Testing
Genetic testing is often recommended to check for mutations that may be driving the overproduction of eosinophils. Identifying specific genetic abnormalities can guide treatment decisions.
Treatments for Hypereosinophilic Syndrome
Treatment for Hypereosinophilic Syndrome focuses on reducing eosinophil levels and preventing organ damage. The choice of therapy depends on the severity of the condition, the organs involved, and whether an underlying cause has been identified.
Medications
Several classes of medications are used to manage Hypereosinophilic Syndrome:
- Corticosteroids: These anti-inflammatory drugs are often the first line of treatment. They help reduce eosinophil production and alleviate symptoms.
- Targeted Therapies: Drugs like imatinib target specific genetic mutations, such as the FIP1L1-PDGFRA fusion gene, and can be highly effective in certain cases.
- Immunosuppressants: Medications like cyclosporine or methotrexate may be prescribed to suppress the immune system and control eosinophil levels.
Monitoring and Follow-Up
Regular monitoring is crucial for patients with Hypereosinophilic Syndrome. Blood tests, imaging studies, and clinical evaluations are performed periodically to assess the effectiveness of treatment and detect any complications early.
Lifestyle Modifications
In addition to medical treatments, lifestyle changes can help manage symptoms and improve overall health:
- Avoiding known allergens or triggers
- Maintaining a healthy diet and exercise routine
- Managing stress through relaxation techniques
Emerging Therapies
Research into new treatments for Hypereosinophilic Syndrome is ongoing. Clinical trials are exploring the use of biologic agents and other novel therapies that target eosinophils more precisely, potentially offering better outcomes with fewer side effects.
Living with Hypereosinophilic Syndrome
Living with Hypereosinophilic Syndrome can be challenging, both physically and emotionally. Patients often require long-term care and support from a team of healthcare professionals, including hematologists, cardiologists, pulmonologists, and dermatologists. Education about the condition and active participation in treatment decisions can empower patients to take control of their health.
Support Networks
Joining support groups or connecting with others who have the same condition can provide valuable emotional support. Sharing experiences and coping strategies can help individuals navigate the complexities of living with Hypereosinophilic Syndrome.