Hydronephrosis, often abbreviated as HN, refers to the swelling of one or both kidneys due to the buildup of urine. This condition occurs when the flow of urine is obstructed or impaired, leading to pressure on the kidneys. While it is not a disease in itself, hydronephrosis is a sign of an underlying problem that requires prompt attention. In this article, we will explore the causes, symptoms, diagnosis, and treatment options for kidney swelling to help you better understand this medical condition.
What is Hydronephrosis?
Hydronephrosis occurs when urine cannot drain properly from the kidney to the bladder. The blockage or obstruction can happen at any point along the urinary tract, which includes the kidneys, ureters, bladder, and urethra. When urine accumulates, it causes the renal pelvis (the central part of the kidney where urine collects) to expand, leading to swelling. If left untreated, this condition can damage the kidney tissue and impair its function over time.
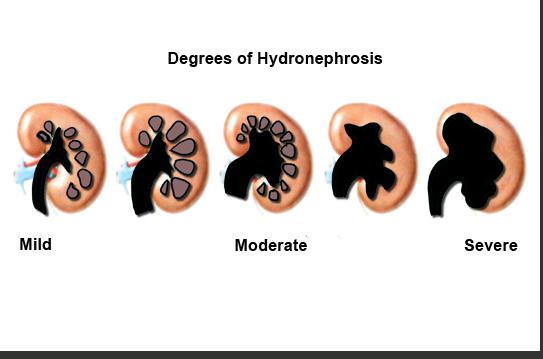
Types of Hydronephrosis
- Unilateral Hydronephrosis: Swelling occurs in only one kidney.
- Bilateral Hydronephrosis: Both kidneys are affected by the swelling.
Causes of Hydronephrosis
The primary cause of hydronephrosis is an obstruction or blockage in the urinary tract. However, there are several factors and conditions that can lead to this issue. Below are some common causes:
Obstruction in the Urinary Tract
An obstruction can occur at various points in the urinary system, including:
- Kidney Stones: Hard deposits made of minerals and salts that form in the kidneys and can block the flow of urine.
- Tumors: Abnormal growths in the urinary tract or nearby areas can press against the ureters or bladder, causing a blockage.
- Blood Clots: Clots can form in the urinary tract and obstruct urine flow.
- Narrowing of the Ureter: A condition known as ureteral stricture can narrow the tube that carries urine from the kidney to the bladder.
Problems with the Bladder
Issues related to the bladder can also contribute to hydronephrosis:
- Bladder Outlet Obstruction: This occurs when the flow of urine from the bladder is blocked, often due to an enlarged prostate in men or pelvic organ prolapse in women.
- Vesicoureteral Reflux: A condition where urine flows backward from the bladder into the ureters and kidneys.
Congenital Conditions
In some cases, hydronephrosis is present at birth due to structural abnormalities in the urinary tract. These include:
- Ureteropelvic Junction Obstruction: A blockage where the ureter meets the renal pelvis.
- Posterior Urethral Valves: Abnormal flaps of tissue in the male urethra that obstruct urine flow.
Symptoms of Hydronephrosis
The symptoms of hydronephrosis can vary depending on the severity of the condition and whether one or both kidneys are affected. Some individuals may experience no symptoms at all, especially in mild cases. However, common signs and symptoms include:
Pain and Discomfort
- Flank pain or discomfort in the side of the body between the ribs and hips.
- Abdominal pain, particularly in the lower abdomen.
- Groin pain that radiates downward.
Urinary Issues
- Frequent urination or the urge to urinate more often than usual.
- Pain or burning sensation during urination.
- Difficulty emptying the bladder completely.
Other Symptoms
- Nausea and vomiting, especially if the condition is severe.
- Fever, which may indicate an infection.
- Swelling or bloating in the abdomen.
Diagnosis of Hydronephrosis
Diagnosing hydronephrosis typically involves a combination of physical examinations, imaging tests, and laboratory studies. Early detection is crucial to prevent complications such as kidney damage or infection.
Physical Examination
A healthcare provider will begin by conducting a thorough physical examination. They may press on the abdomen or flank area to check for tenderness or swelling. The doctor will also review the patient’s medical history and ask about any symptoms they are experiencing.
Imaging Tests
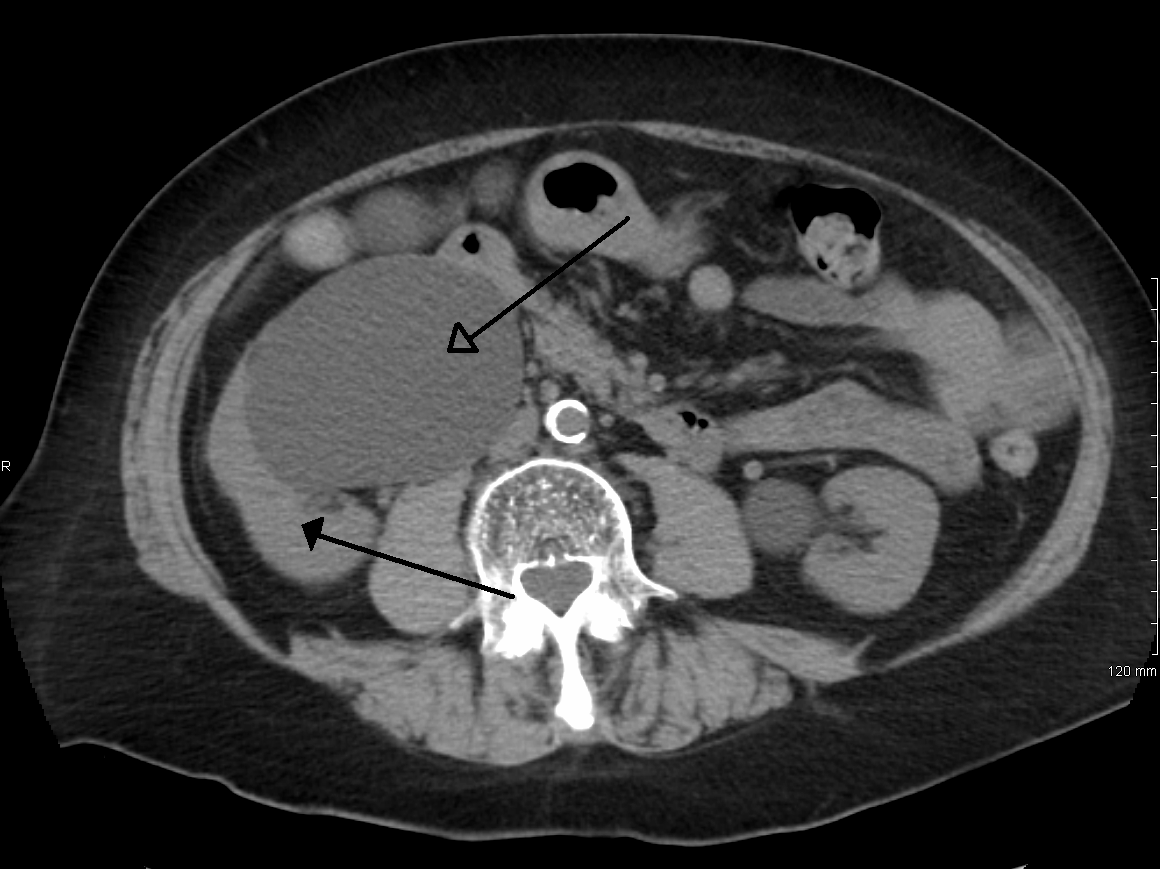
Imaging tests are essential for confirming the presence of hydronephrosis and identifying the underlying cause. Common imaging techniques include:
- Ultrasound: This non-invasive test uses sound waves to create images of the kidneys and urinary tract. It is often the first step in diagnosing hydronephrosis, especially in infants and pregnant women.
- CT Scan: A computed tomography scan provides detailed cross-sectional images of the urinary tract and can help identify obstructions or tumors.
- MRI: Magnetic resonance imaging offers highly detailed images and is particularly useful for evaluating soft tissues and complex cases.
- Voiding Cystourethrogram: This test involves taking X-rays while the bladder is filling and emptying to detect abnormalities such as vesicoureteral reflux.
Laboratory Tests
Blood and urine tests are often performed to assess kidney function and rule out infections. These tests include:
- Blood Tests: To measure levels of creatinine and blood urea nitrogen, which indicate how well the kidneys are functioning.
- Urine Tests: To check for signs of infection, blood, or other abnormalities in the urine.
Treatment Options for Hydronephrosis
The treatment for hydronephrosis depends on the underlying cause, the severity of the condition, and whether one or both kidneys are affected. The primary goal of treatment is to relieve the obstruction, restore normal urine flow, and prevent further damage to the kidneys.
Medications
In some cases, medications may be prescribed to manage symptoms or treat infections associated with hydronephrosis:
- Antibiotics: Used to treat or prevent urinary tract infections.
- Pain Relievers: To alleviate pain and discomfort caused by the condition.
Drainage Procedures
If the obstruction is severe or causing significant kidney damage, immediate drainage of urine may be necessary. This can be achieved through:
- Nephrostomy Tube: A small tube inserted through the skin into the kidney to drain urine directly.
- Ureteral Stent: A thin tube placed inside the ureter to keep it open and allow urine to flow freely.
Surgical Interventions
Surgery may be required to remove or correct the underlying cause of the obstruction. Common surgical procedures include:
- Pyloroplasty: A procedure to widen the ureteropelvic junction in cases of ureteropelvic junction obstruction.
- Tumor Removal: If a tumor is causing the blockage, surgery may be performed to remove it.
- Prostate Surgery: For men with an enlarged prostate, procedures such as transurethral resection of the prostate may be recommended.
Lifestyle Modifications
In addition to medical and surgical treatments, certain lifestyle changes can help manage hydronephrosis:
- Staying well-hydrated to promote healthy urine flow.
- Avoiding foods and beverages that irritate the bladder, such as caffeine and alcohol.
- Managing underlying conditions like diabetes or high blood pressure that can affect kidney health.
Monitoring and Follow-Up
After treatment, regular monitoring is essential to ensure that the condition does not recur and that kidney function remains stable. Follow-up appointments may include repeat imaging tests, blood work, and urine analysis to track progress and detect any complications early.